Conference Schedule
(subject to change)
Nursing CE
This conference is approved for up to 17.00 Nursing CE through the California Board of Nursing.
- Keynote Presentations: 6.00
- Breakout Sessions: 10.00
- Poster Session: 1.00
(2 sessions of 0.50 each, if attending both poster sessions, subtract 0.5 from breakouts)
(pdf)
|
Time
(eastern)
|
Thursday, Nov 3 |
Location |
|
11:30 - 1pm 
|
Lunch & Keynote Address (open to all attendee; Keynote begins at 12noon) 95-R. Which Way is Up? Keeping Well-Being Real and Relevant in a Peri-Pandemic Era
Learner Objectives:
|
199AB |
| 1:15 - 2:15pm |
Breakout 1 69-ASP. Increasing Nurse Leaders Knowledge and Competency in Authentic Leadership
Learner Objectives:
72-R. The Effect of Authentic Leadership and New Graduate Support on New Graduate Nurses Job Satisfaction
Learner Objectives:
|
103A |
| 1:15 - 2:15pm |
Breakout 2 CANCELLED
74-R. Relationships among Mentoring, Empowerment, and Organizational Commitment in Nurse Leaders
Learner Objectives:
|
103B |
| 1:15 - 2:15pm |
Breakout 3 3-R. How COVID-Related Stressors and Work Environment Impact Burnout, Turnover Intention, and Resilience among Nurse Leaders during the Pandemic
Learner Objectives:
|
139 |
| 2:30 - 3:30pm |
Breakout 4 13-R. Presence of Authentic Nurse Leadership during the Pandemic: Two National Studies
Learner Objectives:
23-EBP. Use of Simulation in Developing Nurse Executive Competencies through Executive Rounds (presented by Rebecca (Suzie) Miltner)
Learner Objectives:
|
103A |
| 2:30 - 3:30pm |
Breakout 5 77-QI. Implementing a multimodality, multidisciplinary approach to novice nurse success in the Emergency Department
Learner Objectives:
67-R. Diverse experiences of organizational learning: A grounded theory study
Learner Objectives:
|
103B |
| 2:30 - 3:30pm |
Breakout 6 9-R. The Impact of COVID-19 on Nurse Managers Leadership Characteristics
Learner Objectives:
CANCELLED
|
139 |
|
3:40 - 4:45pm
|
Keynote Address 96-R. KNOW the way, GO the way, SHOW the way: A Chaotic World in Transition
Learner Objectives:
|
199AB |
| 4:50 - 5:20pm |
Poster Session #1 See Poster Tab |
103B |
| 5:30 - 6pm | New Member & First Time Attendee Welcome Reception | South Winter Garden |
| 6 - 7pm | Welcome Reception | South Winter Garden |
| Dorothy Ebersbach Academic Center for Flight Nursing This venue will be open for touring during the opening reception on Thursday from 5-7pm (No tickets required, no food or drink allowed in the center) |
||
| Dinner on your own |
|
Time
(eastern)
|
Friday, Nov 4 |
Location |
|
8 - 9:15am
|
Breakfast & Keynote Address 99-K. Patient Safety & Just Culture
Learner Objectives:
|
153AB |
| 9:30 - 10:30am |
Breakout 7 53-R. Nurse Leader Attitudes and Beliefs on Medical Errors: Supporting Nurses Following a Serious Error
Learner Objectives:
47-QI. Developing Collective Mindfulness Skills in Nurse Leaders to Influence a Culture of Safety
Learner Objectives:
|
103A |
| 9:30 - 10:30am |
Breakout 8 59-EBP. Prevention of CAUTIs in hospitalized adults: An EBP initiative
Learner Objectives:
79-R. Front-line leaders fatigue and cognitive performance: what do we know so far?
Learner Objectives:
|
103B |
| 9:30 - 10:30am |
Breakout 9 Cancelled
26-QI. Baby Its Cold Outside: NICU Post-Op Hypothermia Prevention Bundle
Learner Objectives:
|
189 |
| 10:45 - 11:45am |
Breakout 10 37-R. Nurses Experiences with Change from Nurse-Patient Ratios to Workload Intensity Staffing
Learner Objectives:
33-R. Nursing Staffs Role in Detecting Urinary Tract Infections in Nursing Homes: An Integrative Review
Learner Objectives:
|
103A |
| 10:45 - 11:45am |
Breakout 11 65-EBP. A National Evidence-based Implementation Project Leading Age-Friendly Care in Convenient Care
Learner Objectives:
24-R. Resiliency and Health in Nursing: An Intra-COVID-19 Replication Study
Learner Objectives:
|
103B |
| 10:45 - 11:45am |
Breakout 12 21-R. Supportive Practice Environments Improves Nurse Manager Work-Family Balance and Considerations in a Post-COVID Era
Learner Objectives:
78-R. Improving Work Environment During Persistent Chaos: An Evidence-Based Leadership Approach
Learner Objectives:
|
189 |
| 11:45 - 1:15pm |
Lunch & Case Western Walking Tours Lunch provided by ALSN
|
153AB |
| 1:30 - 2:30pm |
Breakout 13 29-R. Exploring the Relationship Between New Graduate Nurse Psychological Capital and Turnover
Learner Objectives:
34-R. Nurses Burnout, Post-Traumatic Stress, and Stress Biomarker Telomere Length During the Pandemic: Implications for Nurse Leaders
Learner Objectives:
|
149A |
| 1:30 - 2:30pm |
Breakout 14 Poster Session #2 (see Poster 2 tab) |
149B |
| 1:30 - 2:30pm |
Breakout 15 42-EBP. Storytelling as a Pedagogy for Teaching Leadership Competencies
Learner Objectives:
76-R. Facilitating Organizational Resilience During the COVID-19 Pandemic: An Opportunity for Nurse Leaders to Effect a Crisis Leadership Response
Learner Objectives:
|
139 |
| 2:45 - 3:45pm |
Breakout 16 48-QI. Using Branching Scenario Simulations with Graduate Nursing Learners to Support Front-line Nurse Leader Competency Development
Learner Objectives:
71-QI. New Solutions for supporting development of nurse executive presence: Implementation of a graduate level nursing executive presence course.
Learner Objectives:
|
149A |
| 2:45 - 3:45pm |
Breakout 17 49-R. Narrative to Promote Well-Being for Nurse Leaders
Learner Objectives:
46-R. Social Support: Does it Matter to Transformational Leadership Behaviors of Front-Line Nurse Managers? A Mixed Methods Research Study
Learner Objectives:
|
149B |
| 2:45 - 3:45pm |
Breakout 18 60-ASP. The New AACN Essentials - Nursing Education and Leadership
Learner Objectives:
52-ASP. Preparing an Implementation Science-Ready Nurse Leader Workforce
Learner Objectives:
|
139 |
|
4 - 5:15pm
|
Keynote Address 97-K. Research, Nursing, and Innovation: The Triple Helix
Learner Objectives:
|
153AB |
| 5:20 - 6:20pm | ALSN Annual Membership Meeting | 176 |
| Dinner on your own |
|
Time
(eastern)
|
Saturday, Nov 5 |
Location |
|
8 - 9:15am
|
Breakfast & Keynote Address 100-K. Climate Change and Healthcare Disparities: Global Perspectives
Learner Objectives:
|
153AB |
| 9:30 - 10:30am |
Breakout 19 56-QI. Proactive Staffing at the University of Kansas
Learner Objectives:
62-QI. Safe in the Storm or Making Waves? Safe Harbor & High-Stakes Communication
Learner Objectives:
|
103A |
| 9:30 - 10:30am |
Breakout 20 93-R. The Conceptual Model for Professional Identity in Nursing: Academic-Service Implications
Learner Objectives:
31-R. Evaluating the Feasibility of a Mini-Mindfulness Intervention for Nurse Leaders during the Pandemic
Learner Objectives:
|
103B |
| 9:30 - 10:30am |
Breakout 21 16-R. From Dissertaion to Program of Research
Learner Objectives:
86-R. ALSN Relational Leadership Research Collaborative: Relationships among Nursing Leadership Models of Authentic Nurse Leadership and Human-Centered Leadership, and the Transformational Leadership Model
Learner Objectives:
|
139 |
| 10:45 - 11:45am |
Breakout 22 51-R. Women's Power in the Nursing Workplace: A Critical Qualitative Study
Learner Objectives:
82-R. Implementation Sciences Dynamic Sustainability Framework: A Study to Evaluate Alignment with Doctor of Nursing Practice Curriculum and Projects
Learner Objectives:
|
103A |
| 10:45 - 11:45am |
Breakout 23 58-R. Role of Magnet-recognized hospital nurse managers in implementing evidence-based practice: A mixed-method study
Learner Objectives:
70-R. A new framework for rebuilding healthy practice environments: What team virtuousness looks like in healthcare teams
Learner Objectives:
|
103B |
| 10:45 - 11:45am |
Breakout 24 66-ASP. Creating and Evaluating Department-level Budgets
Learner Objectives:
|
139 |
| 12 - 1:00pm |
Breakout 25 68-ASP. Perspectives from Nurse Executives: Understanding Leadership Presence
Learner Objectives:
11-ASP. A Post-Doctoral Program: Enhancing Academic Practice Partnerships
Learner Objectives:
|
103A |
| 12 - 1:00pm |
Breakout 26 22-R. An Exploration of Frontline Nurses Managers Experience during the 2020 COVID-19 Pandemic
Learner Objectives:
|
103B |
| 12 - 1:00pm |
Breakout 27 27-R. Moral Injury, Resilience, and Well-Being among Nurse Leaders during the COVID-19 Pandemic
Learner Objectives:
90-R. Preparing for Realistic Mass Casualty Simulation --Utilizing a Team Leadership Model to bring together UTHealth Academic Leaders and Community Stakeholders
Learner Objectives:
|
139 |
1 - 2:30pm
|
Lunch & Keynote Address 98-R. Nursing the Nation: Extreme Challenges, Extraordinary Impact, 2021 Workforce Survey of Registered Nurses
Learner Objectives:
|
153AB |
| 2:30pm |
Conference Closing |
153AB |
Poster Session #1
(ordered by Abstract ID)
Thursday, Nov 3
4:50 - 5:20pm, Room 103B
5-EBP. Nursing Leadership Mission Critical Checklist
- Angela Prestia, PhD RN NE-BC; Trustbridge/ Florida Atlantic University; Tequesta, Florida
Learner Objectives:
- Recognize the support a checklist can provide to assure the performance of essential processes and eliminate missed opportunities.
- Understand the evidence-based development of each element of the Nurse Leader Mission Critical Checklist.
- The participant will leave with a concrete tool to assist in prioritizing nursing leaders multiple daily challenges.
|
|
25-QI. Bundle It! Implementing Best Practice to Prevent Hypothermia in Neonates Born in L&D
- Tabitha Benga, MSN, BSN, RN, PHN, NE-BC; UCLA Mattel Children's Hospital; Los Angeles, California
- Christine Jiang, RN, BSN, CCRN; UCLA Mattel Children's Hospital; Los Angeles, California
- Siyung Kim, RN, BSN, CCRN; UCLA Mattel Children's Hospital; Los Angeles, California
- Nida Lovatanapongsa, MSN, MSHI CNS CCRN; UCLA Mattel Childrens Hospital; Los Angeles, California
- Anahit Sarin-Gulian, MSN, BSN, RN ABSCN; UCLA Mattel Childrens Hospital; Los Angeles, California
Learner Objectives:
- Recognize elements of a hypothermia prevention bundle. Develop the tools to implement a hypothermia bundle in NICU.
- Understand the importance of standardizing processes and improving knowledge.
|
|
 |
39-R. Nursing Students and New Graduate Nurses Experiences of Psychological Safety: A Longitudinal Study
- Bret Lyman, PhD, RN; Brigham Young University; Provo, Utah
- Charity Cordova; Brigham Young University; Provo, Utah
- Kobe Jensen; Brigham Young University; Provo, Utah
Learner Objectives:
- Describe an effective method for conducting a longitudinal, qualitative study of psychological safety.
- Develop an increased awareness of psychological safetys importance for learning and safe patient care.
- Develop a clearer understanding of the role nurse leaders play in fostering psychological safety.
|
|
 |
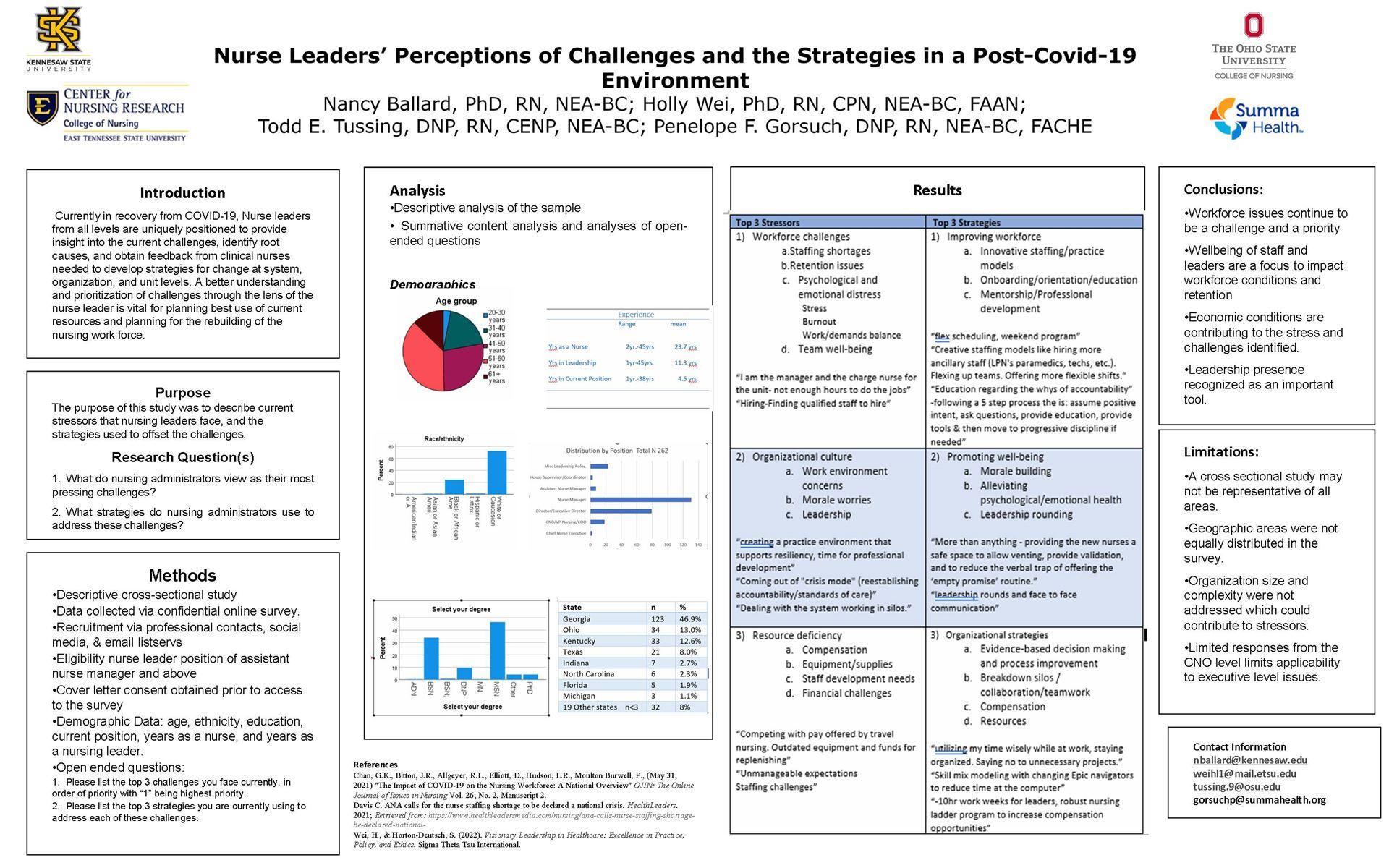
45-R. Nurse Leaders Perceptions of Challenges and the Strategies in a Post-Covid-19 Environment
- Nancy Ballard, PhD, RN, NEA-BC; Kennesaw State University; Kennesaw, Georgia
- Holly Wei, PhD, RN, CPN, NEA-BC, FAAN; University of Louiville; Louisville, Kentucky
- Pennelope Gorsuch, DNP, RN, NEA-BC, FACHE, USAF Col (retired); Summa Health; Akron, Ohio
- Todd E. Tussing, DNP, RN, CENP, NEA-BC; Ohio State University; Columbus, Ohio
Learner Objectives:
- List two current challenges for nurse leaders.
- Identify two current strategies in use to deal with post covid-19 challenges.
|
|
 |
55-QI. Decreasing Delirium with Prevention Interventions in the Intensive Care Unit
- Heidi Karle, BSN, RN; University of Cincinnati and Atrium Medical Center; Fairfield Twp., Ohio
Learner Objectives:
- Learn what delirium means.
- Learn the different types of delirium. Learn at least two ways to try and prevent delirium.
- Learn at least three risk factors for delirium, learn three consequences of delirium.
- Learn how to perform a CAM-ICU assessment as well as a RASS assessment on a patient.
|
|
 |
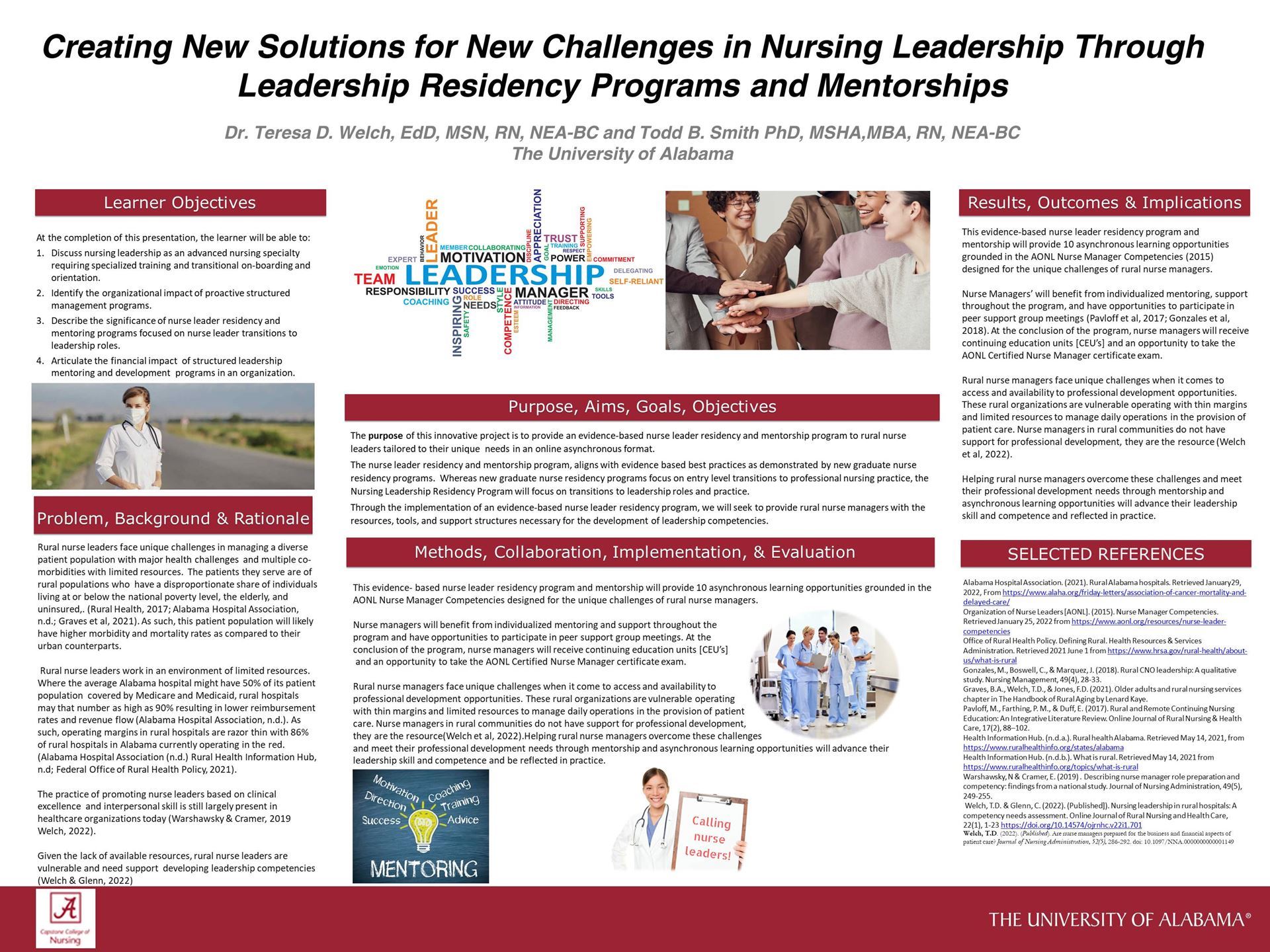
57-EBP. Creating New Solutions for New Challenges in Nursing Leadership Through Leadership Residency Programs and Mentorships.
- Teresa D Welch, EdD, MSN, RN, NEA-BC; The University of Alabama; Tuscaloosa, Alabama
- Todd Smith, PhD, MBA, MSHA, RN, NEA-BC; The University of Alabama; Tuscaloosa, Alabama
Learner Objectives:
- Discuss nursing leadership as an advanced nursing specialty requiring specialized training and transitional on-boarding and orientation. Identify the organizational impact of proactive structured management programs.
- Describe the significance of nurse leader residency and mentoring programs focused on nurse leader transitions to leadership roles.
- Articulate the financial impact of structured leadership mentoring and development programs in an organization.
|
|
 |
63-QI. Keeping "U:" A-Float: Utilizing Information Technology to Disseminate Unit-Specific Practices that Support Float Team Staff Satisfaction
- Adam Fronczek, DNP, RN, MBA, ANP-BC; UCLA Health; Los Angeles, California
- Grace Vargas, RN, BSN, PCCN; UCLA Health; Los Angeles, California
- Sharon Doggett, MSN, RN, B-C; UCLA Health; Los Angeles, California
- Maria Quirch, MSN, RN, OCN; UCLA Health; Los Angeles, California
- Kama Newbry, RN-BC, BSN, PHN; UCLA Health; Los Angeles, California
|
|
 |
73-EBP. Supporting Interim Nurse Manager Role Transition: The Development of an Evidence-Based Toolkit
- Sandra Galura, PhD, RN; University of Central Florida College of Nursing; Orlando, Florida
- Joy Parchment, PhD, RN, NEA-BC; University of Central Florida College of Nursing; Orlando, Florida
- Nora Warshawsky, PhD, RN, CNE, NEA-BC, FAAN; NEW Nurse Leader Solutions, LLC; Corolla, North Carolina
Learner Objectives:
- Understand the phases of interim nurse manager role transition.
- Identify best practices to support and optimize the IM role in each stage of transition.
|
|
 |
80-ASP. Building Community & Sharing Strengths: A Nurse Educator Academic/Practice Collaboration
- Molly Jackson, DNP, MSN, APRN, CNE, ACHPN; Case Western Reserve University; Cleveland, Ohio
- Mary de Haan, MSN, RN, ACNS-BC, CNE; Case Western Reserve University; Cleveland, Ohio
- Michelle Morse, MSN, RN, RN, NPD-BC; University Hospitals Health System in Northeast Ohio; Parma, Ohio
- Holly Ma, MS, BSN, RN, NPD-BC; University Hospitals Health System in Northeast Ohio; Parma, Ohio
Learner Objectives:
- Describe the process of initiating an educational collaboration between academic educators and NPDS.
- Identify two benefits that directly benefit the science of nursing due to academic and practice educator collaboration.
- Identify how nursing leadership is developed as a result of academic and practice educator collaboration.
|
|
 |
81-R. Nurse Acceptance and Use of Continuous Vital Signs Monitoring (CVSM) for Adult Medical/Surgical Patients
- Sarah Knowles, MSN, APRN, ACCNS-AG, GERO-BC, WCC; University Hospitals; Cleveland, Ohio
- Esther Thatcher, RN, PhD; University Hospitals; Cleveland, Ohio
- Mary Anthony, Ph.D., RN; University Hospitals; Cleveland, Ohio
Learner Objectives:
- List the four determinants to acceptance and use of technology.
- Identify the impact of the UTAUT on the acceptance and use of CVSM technology.
|
|
 |
Poster Session #2
(ordered by Abstract ID)
Friday, Nov 4
1:30 - 2:30pm, Room 103B
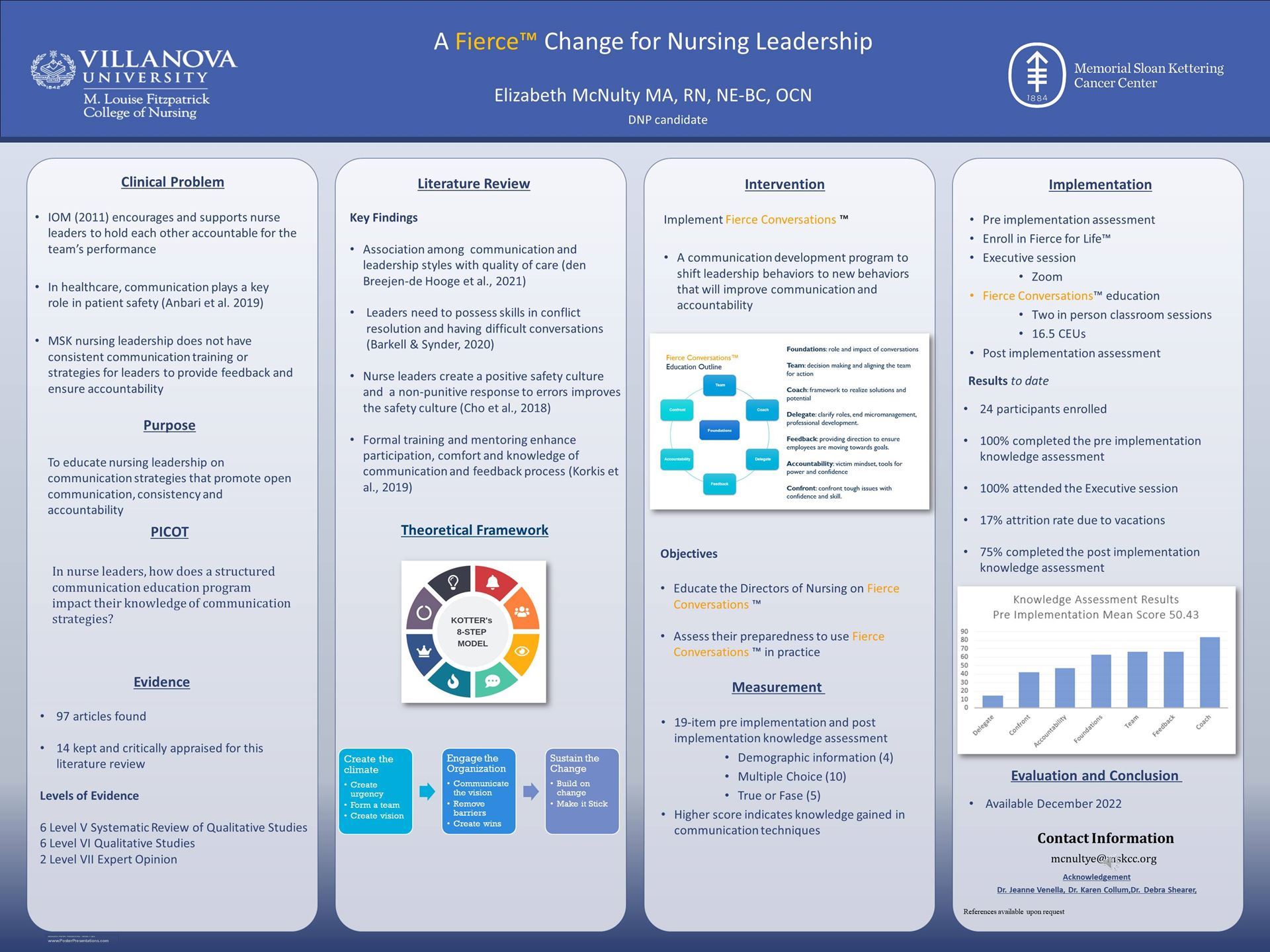
83-EBP. A Fierce Change for Nursing Leadership
- Elizabeth McNulty, MA, RN, OCN, NE-BC; Memorial Sloan Kettering Cancer Center; Northport, New York
Learner Objectives:
- Learn about Fierce Conversations and its ability to transform conversations.
- Understand the value of a structured approach to change in ensuring sustainability.
- Appreciate the role of the nurse leader in culture development.
|
|
 |
89-ASP. Developing Business Skills and Financial Acumen of Nurse Leaders
- Nancy Manning Crider, DrPH, MS, RN, NEA-BC; Cizik School of Nursing at University of Texas Health Science Center at Houston; Houston, Texas
- Marie McBEe, DNP, MSN, RN, NEA-BC; Cizik School of Nursing at University of Texas Health Science Center at Houston; Houston, Texas
Learner Objectives:
- Articulate the requisite business skills, and knowledge of health care economics, health care financing, marketing, and governance/oversight required of DNP and MSN graduates.
- Incorporate learning activities into the graduate nursing curriculum that require the students to utilize quality metrics, financial data, and clinical outcomes to benchmark, plan, budget, and ensure the effective use of resources in the practice setting.
|
|
 |
6-R. Healthcare Workers Health Beliefs Regarding Personal Protective Equipment: A Mixed Methods Study
- Kathleen Morales, PhD, RN, CNE; University of West Georgia; Rome, Georgia
Learner Objectives:
- Describe healthcare workers health beliefs regarding PPE as measured by the Health Beliefs Related to PPE Tool.
- Describe the healthcare workers' calculated risk of infection during the COVID-19 pandemic as measured by the Risk for COVID-19 Infection Tool.
- Describe the relationship between the healthcare workers' calculated risk of infection and their self-reported perceived susceptibility of infection during the COVID-19 pandemic.
|
|
 |
8-ASP. Promoting Excellence in Nurse Leadership: The Coldiron Senior Nurse Executive Fellowship
- Joachim Voss; Case Western Reserve University; Cleveland, Ohio
Learner Objectives:
- Visualize nurse leaders as integral players in the delivery of quality patient care and operational excellence across diverse health care settings.
- Understand the need for nurse executives to catalyze change within individual hospitals and entire health systems.
- Explore the value of an academic-service partnerships through the Coldiron Senior Nurse Executive Fellowship Program example.
- Design similar academic-service partnerships to enhance the development of nurse leaders, the future of nursing and health care.
|
|
 |
10-R. Experience of Travel Nurses during the Pandemic: Results from a National Sample
- Rosanne Raso, DNP, RN, NEA-BC, FAAN, FAONL; NewYork-Presbyterian/Weill Cornell; NYC, New York
- Joyce Fitzpatrick, PhD, MBA, RN, FAAN, FNAP; Case Western Reserve University; Cleveland, Ohio
Learner Objectives:
- Describe the perceptions of travel nurses on their well-being, pandemic impact, work environment and authentic nurse leadership.
- Discuss the implications for nurse leaders of the new world of dynamic staffing models.
|
|
 |
12-R. Clinical nurses view of staffing during the pandemic
- Susan Weaver, PhD, RN, CRNI, NEA-BC; Hackensack Meridian Health; Neptune, New Jersey
- Theresa A. Wurmser, PhD, MPH, RN, NEA-BC; Hackensack Meridian Health; Neptune, New Jersey
- Ulanda Marcus-Aiyeku, DNP, APRN, PMHNP-BC, NE-BC; Hackensack Meridian Health; Neptune, New Jersey
- Joan Harvey, DNP, RN, GERO-BC, CCRN; Hackensack Meridian Health; Neptune, New Jersey
- Kathryn Fleming, PhD, RN, CPHQ, NEA-BC, FACHE; Hackensack Meridian Health; Neptune, New Jersey
Learner Objectives:
- Describe nurses' perspective of staffing during the pandemic.
- Describe recommendations for nurse leaders to institute today and in future emergent events.
|
|
 |
30-QI. Nurse Leaders' Role and Responsibility for Compassion Fatigue
- Kaleigh Sullivan, RN, BSN; University of Rochester; Rochester, New York
- Presentation Handout
Learner Objectives:
- Identify and describe compassion fatigue, burnout, and secondary trauma.
- Apply this knowledge and the researched methods to their specific clinical areas in order to combat these issues.
- Analyze and evaluate the impact of these methods on their nurses by looking into overall staff satisfaction, along with the impacts they have on patient satisfaction and safety outcomes.
- Acquire knowledge, and even courage to create their own environment, and techniques, to prevent and treat compassion fatigue.
|
|
 |
32-R. Profile on New Nurses: A National Perspective in a Post-Pandemic World
- Cory Church, PhD, RN, NPD-BC; Texas Tech University Health Sciences Center; Mansfield, Texas Ryan Schalles, MSN, RN; Texas Tech University Health Sciences Center; Mansfield, Texas
- Presentation Handout
Learner Objectives:
- Explore demographic, education, and employment characteristics of new nurses.
- Identify why new nurses say they want to leave organizations. Examine the reasons why new nurses decide to stay in their positions.
- Relate the reasons why new nurses stay and leave to their own practice settings.
- Investigate possible interventions that may reduce new graduate nurse attrition in their own practice settings.
|
|
 |
35-R. The Implementation of a Neonatal Multiple Patient Simulation in an Undergraduate Nursing Program
- Vuong Prieto, PhD, RN, CHSE; UT Health Houston Cizik School of Nursing; Houston, Texas
- Brandi Virgin, MSN, RN; UT Health Houston CSON; Houston, Texas
Learner Objectives:
- Describe the use of neonatal multiple patient simulation (MPS) in nursing education.
- Discuss the use of unfolding case scenarios in neonatal MPS in nursing education.
- Discuss the benefits of neonatal MPS on BSN nursing students' transition to practice in neonatal nursing care.
|
|
 |
36-R. An Exploration of Nurses Attitudes and Beliefs on Medication Error Reporting Practices: A Qualitative Study
- Andrea Schuermann, MSN, RN, CNML; Orlando Health South Seminole Hospital; Longwood, Florida
- Laura Arkin, MSN, APRN-CNS, ONC, ONC-A, CCNS, FCNS; Orlando Health Orlando Regional Medical Center; Orlando, Florida
- Presentation Handout
Learner Objectives:
- Summarize perceived barriers to medication error reporting. Differentiate between internal and external factors that influence medication error reporting.
|
|
 |
40-R. Organizational learning in healthcare: A systematic review of the literature
- Bret Lyman, PhD, RN; Brigham Young University; Provo, Utah
- Kaitlyn George; Brigham Young University; Provo, Utah
- Sara Frandsen; Brigham Young University; Provo, Utah
Learner Objectives:
- Understand the state of the research related to organizational learning.
- Understand how nurse leaders can better foster organizational learning.
- Understand innovative models and strategies related to organizational learning.
|
|
 |
50-R. Contextual Factors, Mechanisms, and Outcomes of Organizational Learning: An Instrument Validation Study
- Madilyn Jones, BS,RN; Brigham Young University; Provo, Utah
- Natalie Dunkley; Brigham Young University; Provo, Utah
- Bret Lyman, PhD, RN; Brigham Young University; Provo, Utah
Learner Objectives:
- Develop a stronger appreciation for the importance of organizational learning as it relates to quality of care.
- Develop an understanding of two instruments for measuring factors related to organizational learning.
|
|
 |
64-R. Psychometric Analysis of the Critical Thinking Self-Assessment Scale: Identifying, Measuring and Developing Critical Thinking Skills
- Teresa Barry Hultquist, PhD, RN, PHCNS-BC, NE-BC; University of Nebraska Medical Center College of Nursing; Omaha, Nebraska
- Lynnette Leeseberg Stamler, PhD, DLitt, RN, FAAN; University of Nebraska Medical Center College of Nursing; Omaha, Nebraska
- Kevin Kupzyk, PhD; University of Nebraska Medical Center College of Nursing; Omaha, Nebraska
- Louise LaFramboise, PhD, RN; University of Nebraska Medical Center College of Nursing; Omaha, Nebraska
Learner Objectives:
- Recognize the skills and subskills included in the critical thinking conceptual framework and CTSAS.
- Describe the results of the validity and reliability testing and rationale for reduction in tool items.
- Identify possible uses of the revised CTSAS tool in education, leadership, practice, and research.
|
|
 |
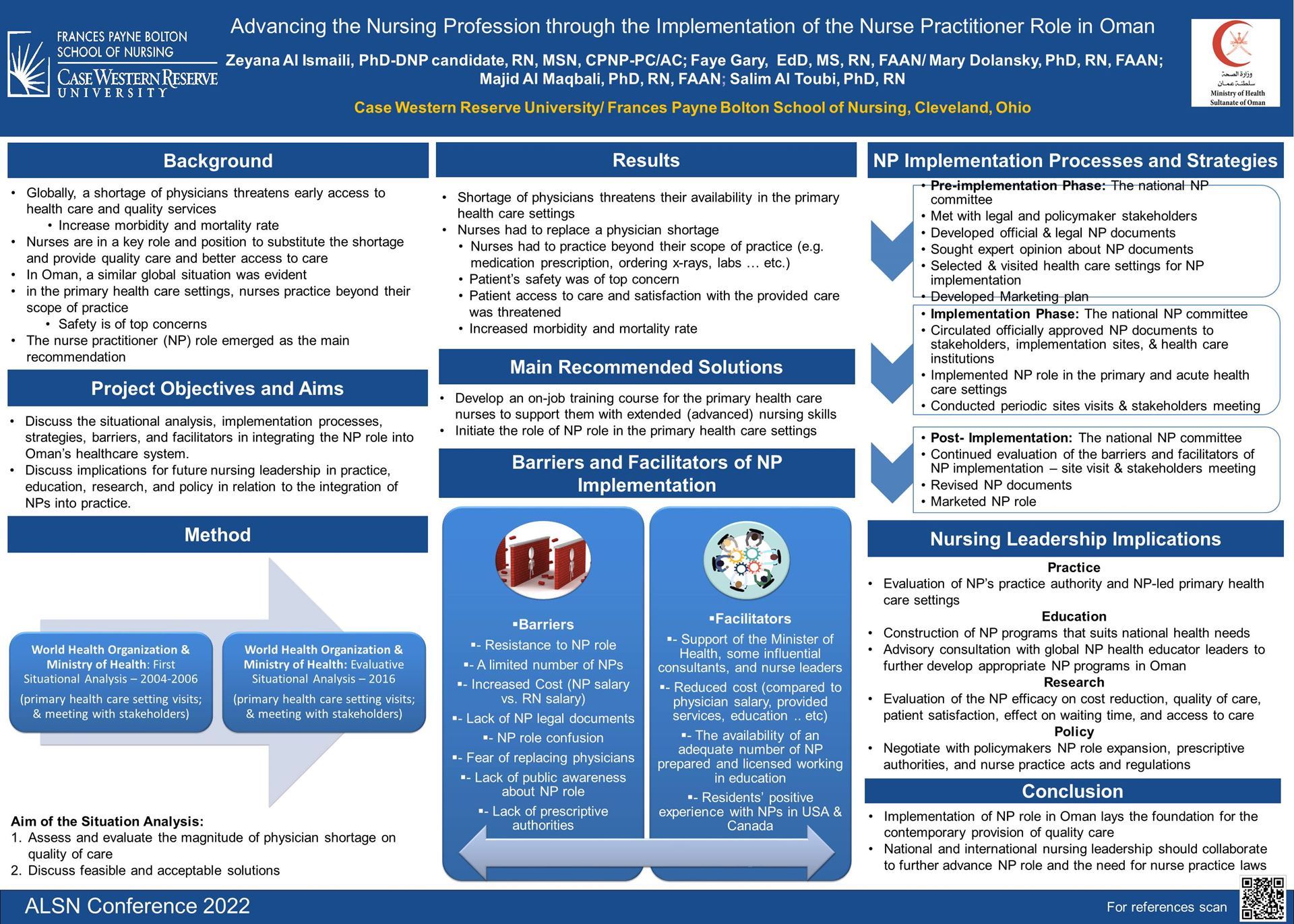
75-QI. Advancing the Nursing Profession through the Implementation of Nurse the Practitioner Role in Oman
- Zeyana Al Ismaili, RN, MSN, CPNP-PC/AC; Case Western Reserve University; Shaker Heights, Ohio
- Faye Gary, EdD, RN, FAAN; Case Western Reserve University, Frances Payne Bolton School of Nursing School of Nursing; Cleveland, Ohio
- Mary Dolansky, RN, PhD, FAAN; Case Western Reserve University; Cleveland, Ohio
- Majid Al Maqbali, RN, PhD, FAAN; Ministry of Healh - Oman; Muscat, Muscat, Oman
- Salem Al Touby, RN, BSN, MSN, PhD; University of Nizwa; Nizwa, Barkat Al Mouz, Oman
Learner Objectives:
- Discuss the implementation processes, strategies, barriers, and facilitators in integrating the NP role into Omans healthcare system.
- Discuss implications for future nursing leadership in research, education, practice, and policy in relation to the integration of NPs into practice.
|
|
 |
84-QI. BUILDING A RESILIENT NURSING WORKFORCE THROUGH HEALTHY WORK ENVIRONMENT (STRESS REDUCTION PROGRAM)
- Rowena Samonte, RN MSN CCRN CNL; VA NORTH TEXAS HEALTH CARE SYSTEM; DALLAS, Texas
Learner Objectives:
- Increase awareness on nursing stress injury and burnout affecting resiliency and patient quality of care.
- Understand the relationship between staff stress and nursing retention.
- Know the importance of healthy work environment to develop a high functioning team.
|
|
 |
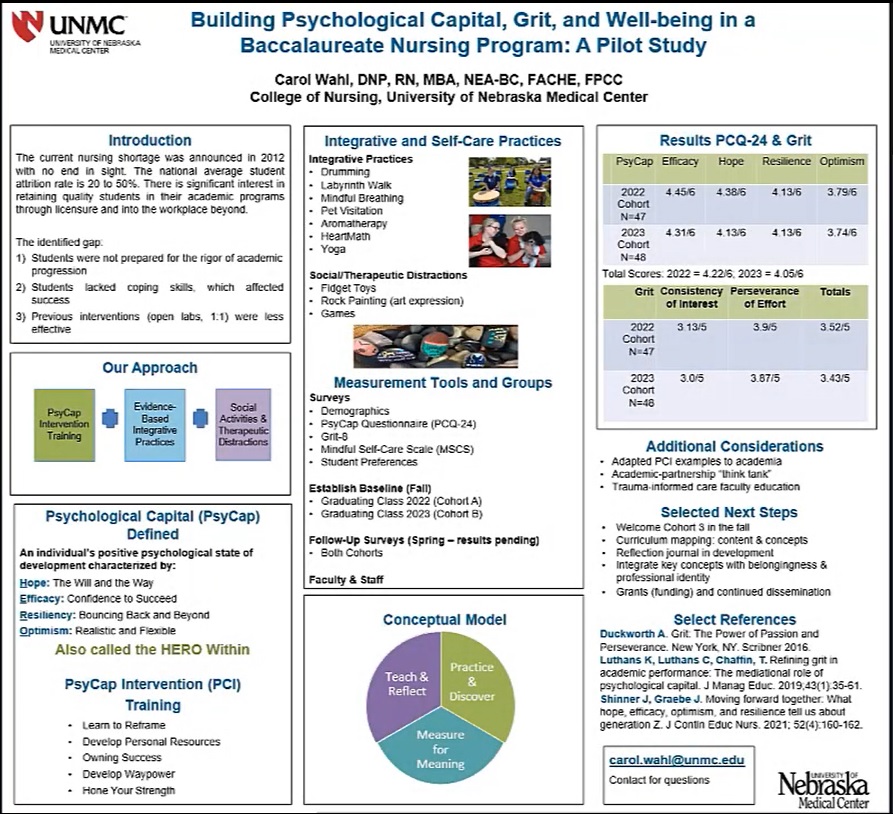
92-EBP. Building Psychological Capital, Grit, and Well-being in a Baccalaureate Nursing Program: A Pilot Study
- Carol Wahl, DNP, RN, MBA, NEA-BC, FACHE, FPPC; University of Nebraska Medical Center; Kearney, Nebraska
Learner Objectives:
- Describe how PsyCap interventions can influence constructs of hope, efficacy, resilience and optimism in facilitating student academic goals.
- Identify how psychological capital and well-being concepts and activities can be successfully integrated within a BSN student curriculum.
- Envision a BSN student retention program utilizing positive psychological capital, grit, and well-being strategies that may support transition into the workforce.
|
|
 |
Presenter Biographies
(ordered by last name)
Delia Abbott, DNP, RN, NPD-BC, NEA-BC, CEN; Texas Tech University Health Sciences Center; Lubbock, Texas
Delia Abbott is currently employed as the Magnet Program Coordinator for Baylor Scott & White Health in the Greater Austin Region. She graduated with a Doctor of Nursing Practice degree from Texas Tech University Health Sciences Center in May 2022. Prior to joining Baylor Scott & White in 2013, Delia worked in the emergency department at hospitals in Shawnee, Oklahoma, and Cedar Park, Texas for 16 years as a staff nurse, charge nurse, clinical coordinator, trauma coordinator, and director. Delia is a member of the following organizations: Texas Nurses Association, American Nurses Association, American Organization for Nursing Leadership, Texas Organization for Nursing Leadership and their Task Force for Regional Clinical Placement, Sigma Theta Tau International, Iota Mu Chapter, and Phi Kappa Phi. She is also an appraiser for the American Nurses Credentialing Centers Pathway to Excellence program.
Arzu Adiguzel, EdD, RN, ACNP-BC, CCRN- CMC, CNEcl; Cos Cob, Connecticut
Dr. Adiguzel has 17 years of nursing as an RN, Acute Care NP and educator in the fields of critical care and emergency. She also served as a preceptor, mentor, instructor and nurse manager. She is a Harvard Macy Scholar. Her dissertation work was dedicated to researching the Impostor Phenomenon in Nurse Leaders.
Larissa Africa, MBA, BSN, RN, FAAN; Versant Center for the Advancement of Nursing; Las Vegas, Nevada
President and CEO of Versant Healthcare Competency Solutions. She has spent almost two decades developing and leading strategies in use of a competency-based transition to practice (TTP) program. This model integrates and standardizes nursing workforce development across the entire healthcare continuum and addresses high-demand areas such as long-term care and home health, including advanced practice nursing, at healthcare organizations nationally. She has published and presented on this topic nationally and internationally.
Rebecca Amrany, RN BSN CPN IBCLC; UCLA Mattel Children's Hospital; Los Angeles, California
Rebecca Amrany has been at UCLA since 2007. She has worked in PICU and NICU. She is a lactation consultant and has taught Baby Basics to NICU parents.
Mary Anthony, Ph.D., RN; University Hospitals; Cleveland, Ohio
Dr. Anthony is Professor Emerita and former Associate Dean for Research at Kent State University and holds the position of Director of Nursing Research and Innovation at University Hospitals Cleveland Medical Center. Her research focus is on linking nursing care delivery with patient, nurse and organizational outcomes and has received funding from federal, national and foundation sources. Dr. Anthony has a strong publication record in top tier journals. She has a successful record of mentoring including serving as Visiting Professor in the U.S. and Brazil. She has held leadership positions in professional and community organizations.
Laura Arkin, MSN, APRN-CNS, ONC, ONC-A, CCNS, FCNS; Orlando Health Orlando Regional Medical Center; Orlando, Florida
Laura Arkin is the Manager of Advanced Practice Providers and the Orthopedic Clinical Nurse Specialist at Orlando Health. She has been with the organization since 2006 and worked as a staff nurse on the Orthopedic Unit at ORMC until she transitioned to her CNS role in 2008. Lauras undergraduate degree is from the University of Florida, holds her Masters from the University of Central Florida and is currently in the PhD program at UCF as well. In 2009, she obtained her green belt in Lean Six Sigma. Laura leads and serves on various multidisciplinary groups which work collaboratively through performance improvement at the local to organizational level to improve the care and outcomes of patients at Orlando Health.
Cynthia Bacon, PhD, RN, CNE, NE-BC; University of NC at Greensboro School of Nursing; Greensboro, North Carolina
Dr. Cindy Bacon is an Associate Professor in the School of Nursing at the University of North Carolina at Greensboro. Her research focuses on the nurses work environment and its effect on nurse and patient outcomes. Her current research project in partnership with Cone Health, and funded by the Duke Endowment for $240,000, examines the effect of workload intensity on nurse and patient outcomes. She is the recipient of more than $18,000 in additional research funding examining nurses' participation in decision making, safety climate and nurse and patient outcomes. Dr. Bacon is the author of nearly two dozen scholarly manuscripts and has presented her work locally, regionally and nationally. Dr. Bacon is an expert educator and enjoys working with graduate students in nursing leadership and research. She also has a background in hospital administration with more than 10 years experience as a nurse leader and is a board-certified nurse executive.
Jacob Bailey, BSN, RN; College of Nursing at The Ohio State University; Columbus, Ohio
Jacob Bailey, BSN, RN is a current doctoral student at The Ohio State University College of Nursing in the Family Nurse Practitioner Program. His four years of nursing experience resides in in pediatric critical care as well as primary care. He also serves as a Graduate Associate with the Ohio State University College of Nursing as a pediatric clinical instructor for pre-licensure students.
K. David Bailey, PhD, MBA, MSN, RN, CCRN-K, NEA-BC, FACHE; UCLA Health; Santa Monica, California
Dr. Bailey serves as the Chief Nursing Officer for UCLA Health Santa Monica Medical Center which is one of the three hospitals within UCLA Health. The Santa Monica campus recently received its second Magnet designation. David serves as a mentor for numerous leaders and staff nurses across the organization and serves as an executive sponsor for several of the local and system-level professional governance model. In addition, Dr. Bailey has been actively engaged in ALSN since 2013 and is currently the President of ALSN. He has served as an invited speaker, panelist, and moderator for various audiences and has published several articles in various professional journals forums. His doctoral work focused on the Examination of Authentic Leadership in Nurse Executives in Magnet and non-Magnet Hospitals.
James Baldwin, MSN, RN, NEA-BC; The Ohio State University Wexner Medical Center; Columbus, Ohio
James Baldwin is a Associate CNO at OSUWMC and a PhD student at OSU CON. Having senior nursing executive leadership responsibilities over the critical care and emergency room areas, he has been on the frontline of the COVID-19 pandemic leading staff RNs, nurse managers and nursing directors. Mr. Baldwins areas of expertise include more than 20-years of clinical care and leadership within emergency and high acuity critical care settings. He has led multidisciplinary teams through strategic expansion and new hospital construction projects. Mr. Baldwin has extensive experience with operational and fiscal stewardship, professional development, team building, change management, quality improvement, psychological safety, and strategic planning.
Nancy Ballard, PhD, RN, NEA-BC; Kennesaw State University; Kennesaw, Georgia
Dr. Ballard an Assistant Professor at Kennesaw State University in Kennesaw, GA, is a Nurse Researcher and Coordinator of the MSN in the Leadership in Nursing-Nursing Administration Track. Prior to her current position, after starting in critical care, she held hospital and system leadership roles as Cardiac Rehabilitation Coordinator, Nurse Manager, Clinical Nurse Specialist, Cardiac Outcomes Coordinator, and Director of the Center for Nursing Excellence for WellStar Health System. Serving as an appraiser and team leader for the ANCC Magnet Designation program for more than a decade has provided insight into excellence in nursing leadership and practice in both national and international settings. Research interest in the practice environment and shared governance has led to presentations of her research at national and international conferences with publications in the American Journal of Critical Care, Journal of Nursing Administration, Journal of Emergency Nursing, Sage and Western Journal of Nursing Research.
Matthew Barroca; Brigham Young University; Provo, Utah
Matthew Barroca, Research Assistant, is currently an undergraduate nursing student in the Brigham Young University College of Nursing, Provo, Utah.
Teresa Barry Hultquist, PhD, RN, PHCNS-BC, NE-BC; University of Nebraska Medical Center College of Nursing; Omaha, Nebraska
Dr. Barry Hultquist is an Associate Professor at the University of Nebraska Medical Center (UNMC) College of Nursing. She holds ANCC certifications as a Nurse Executive and CNS in Public/Community Health Nursing. Her practice background in maternal-child inpatient/clinic settings and home health includes staff, staff development, and nurse leadership positions. She has taught at the undergraduate and graduate level and currently teaches in the MSN Nurse Leader/Executive track and DNP program. She has created e-learning games for common management situations and leads an immersion weekend for management skill development that includes MSN students and practice leaders. She received the 2021 UNMC Academic Affairs/Interprofessional Academy of Educators Impact in Education for Visionary Leadership in Education Award, and 2018 College of Nursing Spirit of Shared Governance Recognition. Dr. Hultquist has been an Evaluator or Project Director on twenty programs, QI projects and/or education grants supported by HRSA and other external funders.
Nimian Bauder, MSN, APRN, AGCNS-BC, NPD-BC, EBP-C; COH; CHATSWORTH, California
Nimian Bauder, MSN, APRN, AGCNS-BC, NPD-BC, EBP-C, has extensive experience in adult-gerontology care as a staff nurse and clinical nurse specialist. She is the clinical nurse specialist (CNS) for the oncology medical surgical units at City of Hope National Center in Duarte, California. As an advanced practice nurse, Mrs. Bauders focus is on improving patient outcomes and ensuring nursing care aligns with up-to-date evidence. Mrs. Bauder graduated with her Bachelor of Science in Nursing in 2009 from Mount St. Marys University in Los Angeles. In 2017, she received her MSN degree with a clinical focus in adult-gerontology care CNS also from Mount St. Marys University. In 2020, she earned her Evidence-Based Practice certificate (EBP-CH) from the Helene Fuld Health Trust National Institute for Evidence-Based Practice in Nursing and Healthcare, which demonstrates her expertise and passion for evidence-based care and quality outcomes.
Pamela Baxter, RN,PhD; McMaster University; Hamilton, Ontario, Canada
Dr. Pamela Baxter has a program of research focusing on examining and developing healthcare leadership to meet the growing demands of healthcare systems provincially, nationally, and internationally. Her research focuses primarily on issues/challenges faced by those providing leadership in long-term, palliative, and end of life care settings. As Co-PI of LEAD Outcomes Research, her goal is to improve outcomes for healthcare leaders, providers, patients, residents and the workplace by synthesizing, disseminating, and generating new knowledge to inform healthcare leader decision making. To achieve this goal, she has engaged in a variety of research projects funded by organizations such as the Canadian Institute of Health Research, the Ontario Ministry of Health and Long-term Care, the Canadian Nurses Foundation, and the Canadian Health Services Research Foundation. Dr. Baxter is a member of ROSA (Research on Organization of Healthcare Services for Alzheimers).
Courtney Benedict, MSN, FNP, CNM, RN; AMN Healthcare; Sonoma, California
Courtney Benedict is a certified nurse-midwife and family nurse-practitioner with over 20 years experience working in a variety of reproductive health and clinical training settings, including Federally-Qualified Health Centers, community hospitals, and private practice. Ms. Benedict has served in reproductive health leadership roles across California, supervising advanced practice clinicians, writing practice guidelines, and has held academic appointments at the University of California, San Francisco, School of Nursing and at Stanford University, Department of Obstetrics and Gynecology.. Ms. Benedict is a doctoral student in Columbia Universitys Doctorate of Education, Nursing where her research focus is on utilizing professional development to grow and retain the health care workforce. Ms. Benedict currently works as the Leader for Clinical Education Solutions at AMN Healthcare.
Tabitha Benga, MSN, BSN, RN, PHN, NE-BC; UCLA Mattel Childrens Hospital; Los Angeles, California
Tabitha Benga is the Quality Manager of UCLA Mattel Children's Hospital. She has previously worked in Quality, Nursing Administration, and clinically as a registered nurse in adult and pediatric critical care. She has a Master's in Nursing Education and a Post-Master's in Nursing Informatics.
Ann Scott Blouin, RN, MBA, PhD, LFACHE; Founder PSQ Advisory & Executive Board Member Institute for Healthcare Improvement; La Grange, Illinois
Believing that quality and patient safety are critical to the strategic success and financial well-being of pediatric health care systems, Dr. Blouin works with senior clinical leadership to help organizations achieve success on financial and clinical metrics through an organizational focus on improvement science and harm avoidance. Ann led the transformation of the survey process at The Joint Commission during her ten year tenure With more than 35 years of health care administration, consulting and clinical maternal/child health nursing experience, Dr. Blouin has held key senior leadership positions at community teaching hospitals, academic medical centers, and prominent global consulting firms. Dr. Blouin earned her PhD in Nursing Sciences and MBA from the University of Illinois at Chicago. She received her MSN with honors from Loyola University of Chicago, and BSN with high honors from Lewis University in Romeoville, Illinois. She is a Lifetime Fellow of the American College of Health Care Executives. She is a certified Green Belt in Lean/Six Sigma/Change Management methodologies. Dr. Blouin has published and presented extensively; she serves as assistant professor on topics for Loyola University’s Marcella Niehoff School of Nursing. Dr. Blouin currently serves on the Boards of the Institute for Healthcare Improvement (IHI) and Ensign Group, a public company focused on post-acute care settings.
Lisa Boss, EdD, PhD, RN, APRN, CNS, CNE; Cizik School of Nursing, UT Health, Houston; Houston, Texas
Dr. Boss received her BSN from the University of Texas Medical Branch at Galveston in 1997. She obtained her MSN as a Clinical Nurse Specialist in Emergency Nursing in 2005 and a post-masters certificate in Nursing Leadership in 2007 from Cizik School of Nursing (CSON), University of Texas Health Science Center, Houston. Dr. Boss completed her PhD in 2013 from CSON and her Doctor of Education in Professional Leadership in Health Science Education in 2022 from University of Houston. Dr. Boss is an associate professor at CSON where she serves as a co-director of the DNP program and teaches in the MSN in Nursing Leadership and the DNP Nurse Executive tracks. Her clinical experience and expertise are focused on emergency nursing, nursing leadership, research, and nursing education. She is passionate about teaching and leading students and nurses.
Susan Campis, MSN, RN, NE-BC; uLeadership; Atlanta, California
Susan Campis has served in progressive leadership roles for over 12 years, her last role being Executive Director, Grady Burn Center, Grady Hospital in Atlanta Georgia. Susan serves as the Chief Health and Wellness Officer providing evidence and inspiration of why nurse leaders must prioritize self-care. As a nurse leader, Susan works to create a safe and healthy work environment where her team can be and perform at their best, ensuring quality care and patient safety.
Deborah Chasco, DNP,CCRN, CNS, APRN; University Medical Center of El Paso; El Paso, Texas
Dr. Deborah Chasco has 22 years of experience in management and administration and 21 years as an advanced practice nurse in the state of Texas with a CNS in maternal child health. She is currently the director of nursing informatics at the University Medical Center of El Paso. She is certified by AACN as a CCRN-E in acute and critical care neonatal nursing. Dr. Chasco teaches at TTUHSC at the Gayle Hunt School of Nursing and mentors informatics students from University of Maryland in Baltimore and Grand Canyon University in Arizona. Dr. Chasco has presented at various national, state, and local conferences. Dr. Chasco has written and been awarded several grants to implement patient care programs and initiatives. She has volunteered on ANIAs Education Committee as Chair, has served as the President of the Southwest Healthcare Executives Association, and is an ANCC Magnet abstract reviewer since 2019 for Magnet Conferences.
Latarsha Cheatham, DNP, RN, APRN, FNP-BC; Cizik School of Nursing, UT Health, Houston; Houston, Texas
Dr. Cheatham is an assistant professor at Cizik School of Nursing, University of Texas Health Science Center, Houston where she teaches in the nurse practitioner, nursing leadership, and DNP programs. Shes an ANCC board-certified Family Nurse Practitioner and Gerontological Nurse. As a NP, shes worked in various settings including, family practice, inpatient, long-term acute care, and retail. She has expertise in quality improvement and have spearheaded innovative processes to improve outcomes and decrease mortality in hospitalized patients. Dr. Cheatham received a BSN from Dillard University in 1998; her MSN as a family nurse practitioner in 2005 from Prairie View A & M School of Nursing. In 2017, she was awarded a DNP from Cizik School of Nursing. Furthermore, Dr. Cheatham completed a post-graduate certificate in nursing education from Cizik School of Nursing in 2020. In her spare time, she enjoys singing and spending time with her family.
ESTHER CHIPPS, PhD, RN, NEA-BC; The Ohio State University; CHARLOTTE, North Carolina
Dr. Esther Chipps holds a dual appointment at The Ohio State University as the Nurse Scientist at The OSU Wexner Medical Center and as a Professor of Clinical Nursing at The Ohio State University College of Nursing. Her research area of interest includes topics related to nursing leadership science and the nursing practice environment. She has been an active member of Association of Leadership Science in Nursing serving as the VP for Research and is currently appointment to the joint Association of Leadership Science in Nursing and Association for Nurse Leaders Foundation Research Advisory Committee. She has been the recipient of numerous research grants and awards including Sigma Theta Tau, AONE and ALSN . She was an the recipient of the March of Dimes Nurse Researcher of the Year in Ohio in 2019 and the Central Ohio Sigma Theta Tau mentorship award in 2017.
Cory Church, PhD, RN, NPD-BC; Texas Tech University Health Sciences Center; Mansfield, Texas
Dr. Cory Church is an Associate Professor at Texas Tech University Health Sciences Center where he teaches in the Traditional Undergraduate Program. Dr. Church has published in the areas of transition to practice and nurse residency programs. He is currently board certified in Nursing Professional Development by the ANCC and serves as a Commissioner for the Commission on Accreditation of Practice Transition Programs at the American Nurses Credentialing Center.
Linda Cole, DNP, RN, APRN, CCNS, CPHQ, CNE, FCNS; Cizik School of Nursing, UT Health, Houston; Houston, Texas
Dr. Cole is an assistant professor at the Cizik School of Nursing at the University of Texas Health Science Center, Houston teaching a variety of courses in both the masters level Nursing Leadership program and DNP program. She serves in a leadership role at CSON as the track coordinator for the Nursing Leadership program and one of four co-coordinators for the Masters in Nursing Programs. She completed her Bachelor of Science degree in Nursing from the University of Southern Mississippi in Hattiesburg, MS. She later completed her Master of Science in Nursing as a clinical nurse specialist along with her Doctor of Nursing Practice from the Cizik School of Nursing. Dr. Cole was inducted as a Fellow in the Clinical Nurse Specialist Institute in 2021. Her interests include integrative medicine, nursing leadership, and nurse resiliency and has published and lectured on these subjects at the local to national levels.
Jeannie Corey , DNP, RN, NEA-BC; James Madison University; Harrisonburg, Virginia
Jeannie Corey, DNP, RN, NEA-BC, Professor of Nursing serves as the Faculty for the Doctor of Nursing Practice program at James Madison University (JMU). Prior to joining JMU, she was faculty at Jefferson College of Health Sciences and Virginia Tech Carilion School of Medicine. She received her Doctorate in Nursing Practice (DNP) from Case Western Reserve University, Masters of Nursing (MSN) from University of Virginia, Bachelors of Science (BSN) in Nursing from Radford University and an Associate Degree (AD) from Virginia Western Community College. She has many years of experience in diverse executive, leadership, clinical and higher education positions. Her research interests are focused on DNP project practices, implementation science, health policy, faculty caring behaviors, moral distress in nurse managers, and interprofessional practice and education.
Nancy Crider, DrPH, MS, RN, NEA-BC; Cizik School of Nursing at University of Texas Health Science Center; Houston, Texas
During my professional career, I have held numerous executive leadership positions in both large tertiary academic medical centers and smaller community hospitals. I hold a BS and MS in nursing, a diploma in accounting and finance, and a doctorate in public health. Currently, I am a fulltime faculty at the University of Texas at Houston, Cizik School of Nursing where I teach leadership, business, and health policy in the DNP Nurse Executive program. I am certified by ANCC (NEA-BC). As an active member of numerous professional organizations, I have served as secretary and board member of TONL, president, treasurer, and board member of HONL, director and treasurer of TNA District 9, and a charter member and treasurer of the American Nursing Informatics Association Houston Chapter. I currently co-chair the TNA/TONL Health Information Technology committee and serve as a representative to the Texas Nursing Legislative Agenda Coalition (NLAC).
Nancy Manning Crider, DrPH, MS, RN, NEA-BC; Cizik School of Nursing at University of Texas Health Science Center at Houston; Houston, Texas
Dr. Crider has held numerous executive leadership positions in both large tertiary academic medical centers and smaller community hospitals. She holds a BS and MS in nursing, a certificate in accounting and finance, and a doctorate in public health. Currently, she is a full-time faculty member at the University of Texas at Houston, Cizik School of Nursing where she teaches leadership, business, and health policy in the DNP Nurse Executive program. She is certified by ANCC (NEA-BC). As an active member of numerous professional organizations, she is currently a board member of the Texas Organization for Nursing Leadership and a member of the ALSN Finance Committee. She is also co-chair of the TNA/TONL Health Information Technology Committee, a member of the TNA Policy Committee, and the HONL representative to the Texas Nursing Legislative Agenda Coalition.
Tim Cunningham, RN, DrPH, FAAN; Emory Healthcare; Atlanta, Georgia
Tim Cunningham, RN, DrPH, FAAN is Co-Chief Well-Being Officer at Emory Healthcare and the Woodruff Health Sciences Center at Emory University. He holds a joint appointment as adjunct associate professor at the Nell Hodgson Woodruff School of Nursing at Emory Healthcare and serves as Vice President of Practice and Innovation for Emory Healthcare. He collaborates with interprofessional teams to support structural and systemic well-being change for healthcare staff and professionals, university staff and faculty, researchers, learners, and community members. Before becoming an executive leader, Cunningham worked as a performing artist and humanitarian clown with organizations such as Clowns without Borders and the Big Apple Circus. He then became and emergency/trauma nurse and practiced clinically for 7 years before completing his doctorate in public health focusing on resilience, well-being, and compassion. Twitter & Instagram: @timcunninghamrn or www.timcunninghamrn.com.
Kimberly Delgado, PhD(c), BSN, RN; East Carolina University; Greenville, North Carolina
Kimberly F. Delgado is a registered nurse, certified dementia practitioner, and a PhD candidate at East Carolina Universitys (ECU) College of Nursing (CON). She has been caring for older adults in skilled nursing facilities for over 18 years, working in various nursing roles, both at the bedside and in leadership positions. Her current research and future research trajectory focus on improving the care of older adults across all long-term care settings. She is a North Carolina Area Health Education Center (NC AHEC) Scholar and a part of the NC Nurses Association Leadership Academy Class of 2022. She is a member of several professional and educational organizations, including the Association for Leadership Science in Nursing, the Beta Nu Chapter of Sigma Theta Tau International Honor Society of Nursing, and ECUs Circle of Omicron Delta Kappa Leadership Honor Society.
Sharon Doggett, MSN, RN, B-C; UCLA Health; Los Angeles, California
Float team clinical nurse manager with 18 years of nursing experience including 7 years in management. Focused on providing excellent compassionate care to patients by supporting our nurses and CNAs in their roles. Has presented at multiple pediatric and leadership conferences in an effort to improve patient care and outcomes. Supported this project by collaborating with our staff members and unit leadership throughout the Health system to improve processes by creating tips sheets to help our staff members feel better prepared to work on over 50 units they float to. This resource can be expanded/modified to help all staff who float.
Mary Dolansky, PhD, RN; CWRU; Ohio
Dr. Dolansky is the Sarah Cole Hirsh Professor of Nursing at the Frances Payne Bolton School of Nursing, Associate Professor School of Medicine Case Western Reserve University (CWRU), Senior Faculty in the Veterans Administration Quality Scholars (VAQS) program at the VA Northeast Ohio Healthcare System, and Nurse Advisor for the national VAQS program. Dr. Dolansky is Director of the QSEN Institute (Quality and Safety Education for Nurses) an international community of healthcare providers with the goal to enhance quality and safety competencies in both academia and practice. She is also Director of the Hirsh Institute which integrates implementation science and practice to improve the quality and safety of healthcare. Her current research includes implementation of the Institute for Healthcare Improvement evidence-based Age-Friendly Health Systems into the 1,100 MinuteClinics across the country and enhancing the role of the RN in primary care through academic-clinical partnerships
Judy Duchscher, RN, BScN, MN, PhD; Thompson Rivers University; Kamloops, British Columbia, Canada
With 4 decades of experience as: a direct care practitioner with a focus in critical care and cardiothoracic nursing, a clinical nurse educator, a college and university professor, a nursing manager and a program coordinator for numerous heart, lung, multi-organ donor and interventional cardiology programs across Canada and the United States, Judys broad range of leadership expertise informs her approach to nursing and her perspectives on the healthcare system. For the past 23 years Dr. Duchscher has been an active researcher, consultant and international leader in the area of new graduate professional role transition the findings of her research have generated a theory of Transition Shock and a model of the Stages of Transition resulting in the publication of more than 20 peer-reviewed articles, 2 books, 13 book chapters and the delivery of over 400 keynotes and workshops throughout Canada, the United States, Australia and Asia on the topic of new nurse integration. In 2003 Dr. Duchscher founded and currently acts as the Director of a federal organization entitled Nursing The Future (NTF) (https://nursingthefuture.ca/) that serves as a bridge between the ideals taught in undergraduate nursing education and the realities of the real world of professional practice. Judy maintains that it is the vision, creativity and passionate commitment of these young professionals, supported by the expert knowledge and practice experience of their senior mentors that will drive nursing and healthcare forward
Cole Edmonson, DNP, RN, NEA-BC, FACHE, FAONL, FNAP, FAAN; AMN Healthcare; Dallas, Texas
Dr. Edmonson has a career spanning three decades with roles from clinical nurse to chief nursing officer, currently he is the Chief Experience and Clinical Officer for AMN Healthcare. He is a Fellow in the American Academy of Nursing, the American College of Healthcare Executives, National Academy of Practice and the American Organization for Nursing Leadership; and Nursing Executive Advanced-Board Certified. He is a Robert Wood Johnson Foundation Executive Nurse Fellow Alum. He completed his BSN and MSN at Oklahoma University College of Nursing and DNP at Texas Christian University.
Sandra Ellingson, DNP, NNP-BC, CPNP; UCLA Mattel Childrens Hospital; Los Angeles, California
Sandra Ellingson is the Nurse Practitioner Supervisor for the NICU, PICU, and PCTICU at UCLA Mattel Childrens Hospital. She holds a Doctorate Degree in Nursing Practice and is dual board certified in both Neonatology and Pediatrics. In addition to her administrative responsibilities, Sandra practices clinically as a Neonatal Nurse Practitioner.
Linda Everett, PhD, RN, NEA-BC,FAAN, FAONL; Case Western Reserve University; Cleveland, Ohio
Dr. Linda Quinn Everett, Visiting Professor Marian K. Shaughnessy Nurse Leadership Academy, Frances Payne Bolton School of Nursing, Case Western Reserve University. From 2007-2015 Dr. Everett served as Executive Vice President and Chief Nurse Executive at Indiana University Health in Indianapolis, Indiana, having previously held the Chief Nursing Officer position at the University of Iowa Hospital and Clinics. In 2007, she was president of the American Organization for Nursing Leadership (formerly AONE). In 2013 she received the National League for Nursing Presidents Award in recognition of her work to strengthen academic-practice partnerships. Dr. Everett received the 2018 AONL Lifetime Achievement Award. She was awarded the University of Michigan School of Nursing Distinguished Alumni award in 2020.
Amany Farag, PhD, RN; University of Iowa-College of Nursing; Iowa City, Iowa
Dr. Farag is a tenured Associate Professor at the University of Iowa College of Nursing. Dr. Farags research goals focus on understanding reactive and proactive approaches to enhance patient safety with emphases on system and human factors contributing to safe care delivery. In her efforts to achieve her research goals, Dr. Farag is currently collaborating with different interdisciplinary teams. They are using machine learning and artificial intelligence to pursue novel approaches to studying measures to contain medication errors and enhance nurses wellness.
Joyce Fitzpatrick, PhD, MBA, RN, FAAN, FNAP; Case Western Reserve UNiversity; Cleveland, Ohio
Dr. Joyce J. Fitzpatrick is Director of the Marian K. Shaughnessy Nurse Leadership Academy and the Elizabeth Brooks Ford Professor of Nursing at the Frances Payne Bolton School of Nursing. Additionally, Dr. Fitzpatrick is a Distinguished University Professor for the Case Western Reserve University. She has published hundreds of papers and books and has presented innumerable times nationally and internationally. Her research interests include leadership, public policy and health care delivery systems. Among many other awards, the Florence Nightingale International Foundation selected her as the recipient of the 2019 International Achievement Award. In 2016 Dr. Fitzpatrick was named a Living Legend of the American Academy of Nursing.
Kathryn Fleming, PhD, RN, CPHQ, NEA-BC, FACHE; Hackensack Meridian Health; Neptune, New Jersey
Kathryn Fleming, PhD, RN, CPHQ, NEA-BC, FACHE, is a Nurse Scientist for Hackensack Meridian Health. She has mentored hospitals and large health systems in quality and performance improvement. She is a testifying expert in the field of Nursing Quality and Informatics. Kathryn is certified as a FACHE, CPHQ and NEA-BC. She earned her MSN in Informatics and PhD in Biomedical Informatics (Healthcare Administration focus) from Rutgers University. She has served on the Board of the New Jersey State Nurses Association and the NJ Legal Nurse Consultant Association. She is the Founder and President of Alliance for Hope a 501(c)(3) charity offering equine therapy to veterans suffering from PTSD. She currently is developing a research study to address the Moral Distress experienced by healthcare workers during the COVID-19 pandemic using equine facilitated learning.
Karen Fowler, Ph.D., RN, CENP; The University of Texas at El Paso; El Paso, Texas
I have been a nurse for over 35 years. The majority of my practice has been in administration. I have been a director of various services then a Chief Nursing Officer of a 400+ acute care facility. I am currently an Associate Professor and director of the post-graduate Master's degree programs of Nursing Administration and Management and Nursing Education.
Nicole Fraire, BSN, RN, CPEN; University Hospital; San Antonio, Texas
Mrs. Fraire earned her baccalaureate degree from Texas A&M Corpus Christi in 2015. She has served in the pediatric ED at University Health System in San Antonio, Texas since 2019. In 2020, Mrs. Fraire became the nurse educator for emergency services. She has dedicated her nursing career to pediatric nursing practice and nursing education. She is an active member of the Emergency Nursing Association. Mrs. Fraire recently presented a poster at the TraumaCon 2022 Conference in Las Vegas, Nevada.
Jihane Frangieh, MSN, RN,; Virginia Commonwealth University; Richmond, Virginia
Ms. Frangieh is an emerging health services researcher with a program of research focusing on the role of nursing leadership in creating and sustaining healthy work environments that produce positive outcomes for patients and staff. She is a seasoned nurse (22 years experience) with a clinical focus in neonatal nursing. She holds an advanced degree (MSN) in nursing administration and is currently a doctoral student at Virginia Commonwealth University in the health care quality and health services research concentration. In addition to her direct care role in Level III neonatal nurseries, Ms. Frangieh has extensive experience in staff development and nursing education. She has designed, implemented, and evaluated leadership development programs for nurse managers and in her current faculty role she integrates leadership content into the masters nursing program at Johns Hopkins University. Ms. Frangieh is a recognized nurse leader and past recipient of the Dorsye Russell Nursing Leadership Fund.
Adam Fronczek, DNP, RN, MBA, ANP-BC; UCLA Health; Los Angeles, California
Adam Fronczek is the director of the Resource Float Team for UCLA Health. Adam joined UCLA in 2013 and served as a staff nurse on the float team, patient placement, and nursing supervisor. In his current role, he is accountable for providing staffing coverage across the health system for inpatient, ambulatory, and procedural settings. Prior to his current role, Adam worked as a nurse practitioner in primary care. He regularly precepts and mentored NP students. His nursing background includes intensive care, perioperative services, and medical-surgical. Adam received his bachelors and Master of Science in nursing from the University of South Florida and his doctorate in nursing practice from Chamberlain College of Nursing. He completed his Master of Business Administration in 2021. Adam is a board-certified adult nurse practitioner and licensed in California. He is a member of the American Organization for Nursing Leadership and the Association of California Nurse Leaders.
Suzanne Gagnon, PhD; University of Manitoba; Winnipeg, Manitoba, Canada
Dr. Suzanne Gagnon, Canada Life Chair in Leadership Education, and Associate Dean, Professional Graduate Programs and Executive Education at the Asper School. In addition to her associate deanship, Dr. Gagnon is the inaugural Director of the James W. Burns Leadership Institute, designing and directing new programming across disciplines including the flagship Presidents Student Leadership Program. Dr. Gagnon conducts seminal research that focuses on identity, inclusion, and leadership development in international firms; leadership and innovation in diverse contexts; and gender equity, representation and strategic change in private and public sector organizations. Her work is published in leading management and organization journals.
Sandra Galura, PhD, RN; University of Central Florida College of Nursing; Orlando, Florida
Sandra Galura, PhD, RN is an Assistant Professor and Director of the Masters in Nursing Leadership and Management program at the University of Central Florida, College of Nursing. With over 30 years of clinical practice, including experience in a variety of clinical and non-clinical leadership roles, her research focuses on issues impacting frontline nursing leadership. She serves on the membership committee of the Association of Leadership Science in Nursing, as a peer reviewer for numerous scholarly journals, and actively contributes to the Continuing the Conversation feature of Nursing Administration Quarterly.
Rocio Garcia, MSN, RN, CNL; University Health; San Antonio, Texas
Ms. Garcia has served as a nurse at University Health System in San Antonio, Texas since 2000 and has been the executive director for emergency services since 2018. Ms. Garcia earned both her baccalaureate and graduate degrees from the University of Texas Health, San Antonio. She has dedicated her nursing practice to the specialty of emergency nursing for over seventeen years. Ms. Garcia has also served as a coordinator for the education committee for the Emergency Nurses Association, adjunct clinical faculty for the University of the Incarnate Word School of Nursing and as a legal consultant.
Rosalie Garcia, RN, BSN, CCRN; UCLA Mattel Children's Hospital; Los Angeles, California
Rosalie Garcia has worked at UCLA since 1996. She has worked as a Trauma ICU RN and CTICU RN and is now the Lead Nurse in the UCLA NICU.
Kaitlyn George; Brigham Young University; Provo, Utah
Kaitlyn George is graduating from Brigham Young University with a BS in Nursing. She has been accepted to multiple nursing graduate programs and anticipates starting graduate studies in Fall 2022. She has co-authored three published articles for peer-reviewed journals, with one additional manuscript in press, and two in preparation.
Dawn Giakas, DBA, MPH, BS, LNHA, CALA, FABC; College of Nursing at The Ohio State University; Columbus, Ohio
Dawn A. Giakas, DBA, MPH, BS, LNHA, CALA, FABC is Administrator of NJ Eastern Star Home, a skilled nursing facility and rehabilitation center, and Lecturer for the College of Nursing at The Ohio State University. She has over 35 years of experience in healthcare, including 25 years as Administrator in post-acute care. Dr. Giakas started her professional career in the Financial Support Division at a Fortune 50 pharmaceutical company. Obtained her MPH degree from the University of Medicine and Dentistry of New Jersey-Robert Wood Johnson Medical School/Rutgers University. Dr. Giakas joined a large, not-for-profit hospital system in the Finance Division, followed by leadership roles in the Long-Term Care Division. She is a licensed nursing home administrator and is certified as an Assisted Living Administrator. She completed doctoral studies in Business Administration at William Howard Taft University and taught business courses including courses in Master of Health Innovation program at OSU.
Nelda Godfrey, PhD, ACNS-BC, RN, FAAN, ANEF; University of Kansas School of Nursing; Kansas City, Kansas
Nelda Godfrey is the associate dean of Innovative Partnerships and Practice at the University of Kansas School of Nursing. A scholar in the area of professional identity in nursing, Dr. Godfrey serves as chair of the International Society for Professional Identity in Nursing. Widely published in innovation and leadership, she is a fellow in the American Academy of Nursing and a fellow in the NLN Academy for Nursing Education.
Pennelope Gorsuch, DNP, RN, NEA-BC, FACHE, USAF Col (retired); Summa Health; Akron, Ohio
Penelope joined Summa Health in November 2021 and provides leadership for ensuring nursing practice and quality standards for all areas of the health system. She is a seasoned healthcare professional with more than 30 years of experience, including 23 years of progressive leadership. She joins Summa Health from The Ohio State University College of Nursing where she led and designed the development of numerous nursing executive leadership courses. Penelope also served as chief nurse executive at Dayton VA Medical Center for two years. Penelope served in and retired from the United States Air Force Medical Service after 28 years where she held numerous leadership roles. Penelope earned a BSN from Brenau Womens College in Georgia, a MSN from University of Nebraska Medical Center and her Doctor of Nursing Practice from Touro University Nevada.
Martha Grubaugh, PhD, RN, NE-BC; Versant Center for the Advancement of Nursing; Las Vegas, Nevada
Martha Grubaugh, PhD, RN, NE-BC has spent almost two decades leading the nursing profession in a variety of managerial and executive positions. Her leadership and research focus has centered on cultivating supportive practice environments for all levels of the healthcare system. Martha is currently the Executive Director of the Versant Center for the Advancement of Nursing (Vcan) and is responsible for strategic and operational management of grant funding, research, and the dissemination of outcomes to advance the nursing profession. She has published and presented regionally and nationally about nursing leadership.
Amanda Haberstroh, PhD, MLIS, AHIP; East Carolina University; Greenville, North Carolina
Amanda L. Haberstroh is Library Assistant Professor at Laupus Health Sciences Library (East Carolina University) where she serves as liaison to the College of Nursing.
Gayle Halas, PhD; University of Manitoba; Winnipeg, Manitoba, Canada
Dr. Gayle Halas is the inaugural Rady Chair in Interprofessional Collaborative Practice, focused on team-based primary health care, and the communication and interactions that enable collaborative practice, particularly for addressing complex needs and care. Her current research explores patient/public/caregiver experiences of team-based care, and transitions in care that are informed by stakeholder experiences and perspectives. She also builds upon collaborative relationships between educational and practice systems and has been actively involved in developing innovative student-infused learning and practice, research capacity building, data resourcing relevant to the broader health workforce and examining leadership strategies and capacity for fostering teamwork within the health care system.
Mikel Hand, EdD, RN, OCN, NE-BC, NEA-BC; University of Southern Indiana; Evansville, Indiana
Dr. Hand is an Professor of Nursing at the University of Southern Indiana. He is also a Research Consultant for Schneck Medical Center in Seymour Indiana. His current research interests consist of three main foci: leadership and health systems, end-of-life care, and curricular innovation. He has a particular interest in resiliency, physical, and mental health among practicing nurses and nursing students.
Joan Harvey, DNP, RN, GERO-BC, CCRN; Hackensack Meridian Health; Neptune, New Jersey
Joan Harvey, DNP, RN, GERO-BC, CCRN, a nurse scientist at Hackensack Meridian Health Ann May Center for Nursing, has more than 38 years of nursing experience in both the clinical setting and nursing education. Joan has participated in various research studies ranging from nurses' attitudes regarding restraint use, spirituality and nursing, bedside reporting to joint work with her colleagues regarding teamwork and care of older adults.
Margot (Lisa) Hedenstrom, PhD, RN, MSN, MBA, NEA-BC; Kennesaw State University; Kennesaw, California
Dr. Hedenstrom is an Assistant Professor at Kennesaw State University where she teaches in the MSN Nursing Administration track. She is certified as a Nurse Executive Advanced from the American Nurses Credentialing Center. Prior to joining Kennesaw State, she worked for many years in system and organizational nursing executive leadership roles. She has a BSN from Georgia Southern University, a MSN from Medical College of Georgia, a MBA from Brenau University, and a PhD in Nursing from Georgia State University. She has presented nationally and published in Mentoring and Developing Nurses and Nurse Leaders. Her research interests include developing and mentoring nursing students, nurses, and nurse leaders. She is currently working on research projects and work in mentoring clinical nurses and mentoring nurse leaders for team trust.
Margot Lisa Hedenstrom, PhD, RN, MSN, MBA, NEA-BC; Kennesaw State University; Kennesaw, Georgia
Dr. Hedenstrom is an Assistant Professor at Kennesaw State University where she teaches in the MSN Nursing Administration track. She is certified as a Nurse Executive Advanced from the American Nurses Credentialing Center. Prior to joining Kennesaw State, she worked for many years in system and organizational nursing executive leadership roles. She has a BSN from Georgia Southern University, a MSN from Medical College of Georgia, a MBA from Brenau University, and a PhD in Nursing from Georgia State University. She has presented nationally and published in Mentoring and Developing Nurses and Nurse Leaders. Her research interests include developing and mentoring nursing students, nurses, and nurse leaders. She is currently working on research projects and work in mentoring clinical nurses and mentoring nurse leaders for team trust. She serves as Pathway To Excellence Appraiser and team leader since 2010, and also serves as a Magnet Appraiser since 2018 for the ANCC.
William Herrera, MSN, RN, CEN, CFRN, CCRN, TCRN; University Hospital; San Antonio, Texas
William Herrera MSN, RN, CEN, CFRN, CCRN, TCRN is an educator in the Emergency Department at University Hospital in San Antonio, TX. His passion for emergency and trauma nursing has evolved into the desire to educate colleagues in the same. He graduated with honors with his Master of Science in Nursing from Grand Canyon University in 2019. He remains an active member in several national committees: Emergency Nurses Association, Air & Surface Transport Nurses Association and American Association of Critical Care Nurses. He is also a member of Sigma Theta Tau National Honor Society. William is certified in emergency, flight, critical care, and trauma nursing. He has served as Medical Crew Lead for Methodist Aircare and Patient Care Coordinator for the Trauma Resuscitation Unit in the Emergency Department at University Hospital and Adjunct Faculty for the University of The Incarnate Word Nursing Program.
Katherine Huefner, SN; Brigham Young University College of Nursing - Provo, UT; Provo, Utah
Katie is a student nurse and research assistant at BYU. She will graduate in April 2023.
Marjorie Jenkins, PhD, RN, NEA-BC, FACHE; Cone Health; Greensboro, North Carolina
Dr. Marjorie Jenkins is the director of nursing research at Cone Health in Greensboro, North Carolina. She is a co-investigator on the Duke Endowment study examining the effect of workload intensity on nurse and patient outcomes.
Christine Jiang, RN, BSN, CCRN; UCLA Mattel Children's Hospital; Los Angeles, California
Christine Jiang has worked as a clinical nurse in the UCLA Mattel Childrens Hospital NICU for the past 12 years. She obtained her Baccalaureate in Science of Nursing from UCLA SON. She is currently the co-chair of the NICU Hypothermia Taskforce.
Terry Jones, PhD, RN; Virginia Commonwealth University; Richmond, Virginia
Dr. Jones is a health services researcher with a program of research focusing on the nurse workforce and nursing care quality in acute care environments. She has advanced degrees in nursing (MSN), clinical sciences (MS) and research (PhD). She is a tenured associate professor at Virginia Commonwealth University where she serves as the concentration lead for the nursing leadership and organization science masters program and lead faculty in the healthcare quality/health services research doctoral program concentration. Dr. Jones has experience as a nurse leader/administrator in an academic medical center and continues as a consultant on workforce and care delivery issues. She has completed research related to staffing trends, academic preparation of the nurse workforce across the continuum of care, leadership development among direct care nurses, and the prevalence and patterns of unfinished (missed) nursing care. She has authored 45+ peer reviewed publications and has presented her research at numerous conferences.
M. Lindell Joseph, PhD, RN, FAAN, FAONL; The University of Iowa College of Nursing; Iowa City, Iowa
Dr. Joseph is a Clinical Professor and the Director of the Health Systems/Administration and CNL Programs at the University of Iowa College of Nursing. In addition, she is a Councilor on the Faculty Senate at the University of Iowa. She currently serves on the American Organization for Nursing Leadership (AONL) Foundation Board of Directors and on the Advisory Council for International Society for Professional Identity in Nursing (ISPIN). She is a fellow in both the American Academy of Nursing and The American Organization for Nursing Leadership. Dr. Josephs area of expertise is innovativeness, leadership effectiveness, and the General Effectiveness Multilevel Theory for Shared Governance (GEMS), the only theory-based program for shared governance in nursing practice.
Heidi Karle, BSN, RN; University of Cincinnati and Atrium Medical Center; Fairfield Twp., Ohio
I have worked in the ICU since I graduated nursing school 16 years ago. I am very passionate about critical care patients and mental health. I am currently in the Psych Mental Health Nurse Practitioner program at the University of Cincinnati and graduate in August. I am looking forward to being able to help clients to improve their mental health. I currently reside in Fairfield Township, Ohio with my boyfriend and my two daughters.
Kay Kennedy, DNP, RN, NEA-BC, CPHQ; ULeadership, LLC; Altanta, Georgia
Dr. Kay Kennedy is a Human-Centered Leader, author, nurse educator, and entrepreneur. She teaches in the DNP program at Emory University and holds an adjunct faculty appointment at Mass General Hospital Institute of Health Professions. She is the Chief Executive Officer of ULeadership, LLC. By combining a love for nurses, patients, and quality improvement, she has led large nursing teams to create healthy work environments, satisfied patients, and consistent, high-quality care. Dr. Kennedy has held multiple leadership roles from the bedside to Chief Nursing Officer. Her goal as a leader is to ignite innovative problem-solving; develop others to be their best; and lead by serving others.
Minjin Kim, PhD, RN; University of Cincinnati; Cincinnati, Ohio
Dr. Minjin Kim is a tenure-track Assistant Professor at the University of Cincinnati (UC). She is dedicated to reducing health disparities, improving health promotion and disease prevention, and advancing innovation using human-centered interventions to improve health and reach underserved, high-need populations. Promoting health equity and understanding the root causes of health disparities has emerged for her as a powerful and rewarding pathway. In particular, she has acquired specific expertise with the intervention modality of storytelling as interventions that leverage technologies (i.e., digital health, mHealth, chatbot) to enhance health communication with racial, ethnic, and minority populations. She is a co-editor and an author of the book titled The 1.5 Generation Korean Diaspora: A Comparative Understanding of Identity, Culture, and Transnationalism. Dr. Kim is a KL2 scholar through the Center for Clinical & Translational Science & Training at the UC and has recently been selected for the Association for Leadership Science in Nursing Foundation Pilot Award.
Siyung Kim, RN, BSN, CCRN; UCLA Mattel Children's Hospital; Los Angeles, California
Si is a clinical nurse III at UCLA Mattel Childrens Hospital. She has been working in Neonatal Intensive Care Unit as a bedside, relief charge and resource RN. She has CCRN Neonatal Certification. She has Bachelor's degree in Biological Sciences from Rutgers University and Associate of Science in Nursing from UMDNJ.
Patricia Kinser , PhD, WHNP-BC, RN, FAAN; Virginia Commonwealth University; Richmond, Virginia
Dr. Patricia Kinser is an Endowed Professor and Assistant Dean of Research, Scholarship, and Innovation at the Virginia Commonwealth University (VCU) School of Nursing. Her biobehavioral program of research is focused on mental health in women across the lifespan. The main focus of Dr. Kinsers work is to examine non-pharmacologic symptom prevention and management strategies for depression and related symptoms, using her expertise in integrating biologic, quantitative, and qualitative data. She is the principal investigator of several NIH-funded studies: the Mindful Moms Study, the Mamma Mia Study, and the LEGACI Study. Dr. Kinser is a Fellow of the American Academy of Nursing and a governor-appointed member of the Commonwealth of Virginia Board of Health. She maintains an active clinical practice as a Womens Health Nurse Practitioner at a local free clinic in Richmond, VA.
Sarah Knowles, MSN, APRN, ACCNS-AG, GERO-BC, WCC; University Hospitals; Cleveland, Ohio
Sarah is a Clinical Nurse Specialist (CNS) in acute care at University Hospitals. Sarah works to improve patient outcomes by providing direct patient care and expert consultation, ensuring nursing care is scientifically-based and up-to-date and educating nurses and the health care team about new research, practice, innovations, interventions, and procedures. Sarah earned a MSN in nursing education at Cleveland State University and a post Masters certificate as an Adult/Gero CNS from Kent State University. She is currently enrolled in the Doctor of Nursing Program at Ursuline College. Sarah is certified in gerontological nursing and wound care, as well as, as an adult/geriatric CNS in wellness through acute care. Since 2016, Sarah has led initiatives to design and implement the CVSM training and mentoring for nursing practice. She serves as an expert on UHs Continuous Cardio-Pulmonary Monitoring ERM committee and as a regional ambassador for the Patient Safety Movement Foundation (PSMF).
Dana Koziol, MSN, RN, BA; Creighton University; Omaha, Nebraska
Dana Koziol received an MSN in leadership from Nebraska Wesleyan University. She is currently a faculty in the undergraduate traditional BSN program and ABSN program at Creighton University College of Nursing. Dana has been a registered nurse since 2009 working in inpatient mental health settings with geriatric, adult, and pediatric mental health patients. She has also been involved in several levels of leadership through hospital shared governance and participated in supervisory roles in hospital settings. Dana is currently a student at the University of Kansas Medical Center in the Post-Masters Doctor of Nursing Practice- Leadership program. Her teaching and future research interests include; leadership development, moral distress in nurses and nurse managers, and care delivery models.
Kevin Kupzyk, PhD; University of Nebraska Medical Center College of Nursing; Omaha, Nebraska
Kevin A. Kupzyk is an assistant professor and statistician at the University of Nebraska Medical Center. He received his training in quantitative methods in education at the University of NebraskaLincoln, and his research interests include multivariate statistics, assessment, longitudinal methods, structural equation modeling, latent growth curve modeling, power analysis, and multi-level modeling (mixed modeling). His duties involve teaching quantitative methods and statistical consulting, including data cleaning, database management, performing and interpreting quantitative analyses and collaborating in writing and preparing manuscripts for publication. He has extensive experience in assessing the psychometric properties of scales, is adept at handling large datasets, and working with longitudinal data from intervention studies.
Louise LaFramboise, PhD, RN; University of Nebraska Medical Center College of Nursing; Omaha, Nebraska
Dr. LaFramboise, Associate Professor and Assistant Dean at the University of Nebraska Medical Center (UNMC) College of Nursing was previously Director of the Baccalaureate Program. She noted students struggled with critical thinking in classroom and clinical settings. In service to the Nebraska State Board of Nursing, Dr. LaFramboise realized UNMC students were not alone in their critical thinking challenges. Recognizing the need for action, Dr. LaFramboise and colleagues sought to identify a valid and reliable tool to measure critical thinking in undergraduate nursing students as a first step in the process of more fully developing critical thinking ability in pre-licensure nursing students. In recognition of her academic accomplishments, in 2016 Dr. LaFramboise was an inaugural inductee into the UNMC Interprofessional Academy of Educators and in 2019 received the Virginia Tilden Leadership Award. She has been project director on three HRSA grants focused on developing innovative educational programs.
Lucy Leclerc, PhD, RN, NPD-BC; uLeadership; Atlanta, Georgia
Dr. Lucy Leclerc is an experienced researcher, executive leader, author, and frequent speaker to large healthcare groups from local to global audiences. Dr. Leclerc's expertise and research focus on the connection between relational leadership approaches and outcomes such as the AACN Healthy Work environment standards.
Jennifer Ledlow, MSN, RN, CCRN-K, CNL, CNE; University of Alabama at Birmingham; Birmingham, Alabama
Jennifer Ledlow received her BSN and MSN degrees from the University of Alabama at Birmingham (UAB) School of Nursing. She has over 17 years of nursing experience in a variety of settings, including medical/surgical, hospice, critical care, and administration. Ms. Ledlow is the UAB SON Nursing Simulation Coordinator and an Instructor.
Lynnette Leeseberg Stamler, PhD, DLitt, RN, FAAN; University of Nebraska Medical Center College of Nursing; Omaha, Nebraska
Dr. Stamler is Professor and Associate Dean for Academic Programs at the University of Nebraska Medical Center (UNMC) College of Nursing. She has taught or practiced nursing in five states and three Canadian provinces. She has taught nursing from diploma programs to doctorate. Her research interests are eclectic but all contain an aspect of teaching and learning, whether patient or student centered. Dr. Stamler served on the Board of Directors of the Canadian Association of Schools of Nursing for several years, culminating in the presidency (2008-2010). She was inducted into the American Academy of Nursing in 2011 and received the 2018 UNMC Academic Affairs/Interprofessional Academy of Educators Impact in Education for Visionary Leadership in Education Award. She has served as an accreditation site visitor in both U. S. and Canada and is the founding co-editor of the undergraduate text Community Health Nursing: A Canadian Perspective.
Lori Loan, PhD, RN, FAAN; University of Alabama at Birmingham; Birmingham, Alabama
Dr. Lori A. Loan, PhD, R.N., FAAN is the Director of the Executive Doctorate in Nursing Practice Program and an Associate Professor at the University of Alabama at Birmingham, U.S.A. She received her BSN degree from Pacific Lutheran University and her M.S. and PhD degrees from the University of Washington, School of Nursing in Seattle. Her post-doctorate education includes Advanced Leadership credentials from the U.S. Army Management Staff College and a Lean Six Sigma Black Belt from the U.S. Army Office of Business Transformation. Many of Dr. Loan's significant contributions resulted in the transformation of nursing practice and policy through effective mentorship, leadership, and the infusion of evidence-based practice. She has extensive experience as an investigator and consultant on studies and evidence-based practice projects with funds totaling over 8 million dollars. Dr. Loan has mentored more than 35 nurses who completed over 50 national and international grant-supported projects and studies.
Figaro Loresto Jr, PhD, RN; Versant Healthcare Competency Solutions; Las Vegas, Nevada
Figaro L. Loresto Jr, PhD, RN is a biostatistics consultant for Versant Healthcare Competency Solutions. Additionally, he is a nurse scientist at Childrens Hospital Colorado and Assistant Professor at the University of Colorado College of Nursing. Figaro is a trained biostatistician obtaining a doctoral degree in Clinical Science with a concentration in biostatistics. His main area of interest is health services research, network analysis, and text mining methodologies.
Lyn Losty, PhD, MBA, RN; Walden University; Minneapolis, Minnesota
Marilyn (Lyn) has had a strong career in today’s healthcare environment. Starting as a surgical intensive care nurse, she practiced clinically for over 5 years, spent 10 years in executive leadership at Hill-Rom Industries and culminated her career with 18 years in higher education at the University of Maryland School of Nursing (UMSON) where she served as an associate professor and Director of the Health Services, Leadership, and Management specialty track. Currently, Lyn is a contributing faculty member in Walden University School of Nursing’s DNP and PhD programs where she teaches and mentors tomorrow’s nurse leaders. Lyn holds a PhD from the University of Maryland Baltimore County in Public Policy; an MS from the University of Maryland School of Nursing; an MBA from the University of Baltimore, and a BSN from Carlow University in Pittsburgh, PA.
Nida Lovatanapongsa, MSN, MSHI CNS CCRN; UCLA Mattel Childrens Hospital; Los Angeles, California
Nida Lovatanapongsa is the Clinical Nurse Specialist in the NICU at UCLA Mattel Childrens Hospital. She has been at UCLA since 2007. She has clinically practiced as a registered nurse in the neonatal intensive care unit and pediatric ECMO team. She has a Master in Nursing and Health Informatics.
Shelly Luger, RN, DNP, NE-A; Creighton University; Omaha, Nebraska
Dr. Shelly Luger received a DNP in Organizational Leadership and a Certificate in Health Professions Education from The University of Kansas Medical Center. She is currently the Track- Lead for the Nursing Administration and Leadership graduate tracks a Creighton University College of Nursing. Dr. Luger has held several leadership positions in nursing and nursing education. She participated in a health policy residency program supported by the Department of Health and Human Services, Agency on Healthcare Research and Quality, and the United States Preventative Services Task Force. She is an Evidence-Based Practice mentor and has orchestrated student cultural immersion and service-learning opportunities on the Rosebud Reservation. Dr. Lugers current project interests include developing leadership skills in new graduate nurses, complexity science, narrative nursing leadership, and systems leadership in free and charitable clinics.
Bret Lyman, PhD, RN; Brigham Young University; Provo, utah
Bret Lyman, PhD, RN, is an Associate Professor of Nursing at Brigham Young University, Provo, Utah. He earned a PhD in nursing from the University of Northern Colorado, minoring in Applied Statistics and Research Methods. He studies organizational learning in hospitals. His published work provides guidance for researchers and nurse leaders who are committed to empowering healthcare teams and improving clinical outcomes.
Ulanda Marcus-Aiyeku, DNP, APRN, PMHNP-BC, NE-BC; Hackensack Meridian Health; Neptune, New Jersey
Ulanda Marcus-Aiyeku, DNP, APRN, PMHNP-BC, NE-BC, a nurse scientist at Hackensack Meridian Health (HMH) has 25 years of experience in leadership roles across the care continuum. Dr. Aiyeku is a board certified psychiatric advanced practice nurse with a body of research that is grounded in inquiry to the social determinants of health. Her recent work includes a multi-center investigation of perceived mental health and postoperative outcomes in patients undergoing total joint replacement surgery. Aiyeku represents HMH as an advisory board member and mentor for the HRSA ANE- Fellowship Grant for entry level APNs working in underserved communities.
Della Mathew, PhD, PGDHA, EDHI, RN; Memorial Hermann Texas Medical Center; Houston, Texas
Dr. Della Mathew is the Clinical Nurse Educator of Neuroscience ICU & Neuro Vascular ICU of Memorial Hermann Hospital at Texas Medical Center. Recently she received her Ph.D. in Nursing Science from Texas Womans University, Houston. Her masters in nursing is from Irish, and bachelors is from Indian Universities. The academic degrees add diplomas in hospital administration and healthcare informatics. Dr. Mathew is a Nurse for 25 years with solid ICU background. She worked in three different countries, and roles extended from registered nurse to policy and procedure development, education, and research. She received several professional awards and research grants. As a dedicated nurse professional, Dr. Mathew like to advance her roles in education and research to promote evidence-based practice and nursing scholarship. Currently, Dr. Mathew lives in Houston with her husband and two sons. She believes in life-long learning, but a lot of her time is taken for cooking!
Marie McBEe, DNP, MSN, RN, NEA-BC; Cizik School of Nursing at University of Texas Health Science Center at Houston; Houston, Texas
Dr. McBee has held numerous leadership nursing leadership positions. She received her DNP degree from the University of Alabama Birmingham. She currently teaches full-time in the MSN and DNP programs at Cizik School of Nursing, Houston, TX.
Deborah McCrea, EdD, APRN, FNP-BC,CNS, CEN, CFRN, EMT-P; UTHealth School of Nursing at Houston; Houston, Texas
Debbie McCrea is an assistant professor at UT-Health Houston where she teaches in the family and emergency nurse practitioner program. She completed her masters degree in the Emergency CNS/Education and postmasters certificate in the Emergency Nurse Practitioner program and Family Nurse Practitioner program at UT. She was a prehospital Clinical Nurse Specialist at the Houston Fire Department and a fixed wing flight nurse. She also taught EMS for 15 years at Houston Community College. Dr. McCrea also works part time as a medical case manager for a travel assistance company coordinating care for domestic and international travelers including setting up emergent air evacuation for clients who experience medical and trauma emergencies. She recently completed an Educational Doctorate (EdD) in Professional Leadership in Health Science Education from the University of Houston where her interest includes instructional technology and educational simulation especially in Mass Casualty Training.
Tracy McKinney, BSN, RN, CHPN; Schneck Medical Center; Seymour, Indiana
Tracy is a Hospice Case Manager at Schneck Medical Center. She became interested in the topic of resiliency during completion of the Nurse Residency Program. She is particularly interested in resiliency as a way to understand the phenomenon of burnout in her specialty and in the nursing profession as a whole.
Elizabeth McNulty, MA, RN, OCN, NE-BC; Memorial Sloan Kettering Cancer Center; Northport, New York
Elizabeth is the Director of Acute Care Nursing at MSK. She earned her BSN from Binghamton University, MA in Nursing Administration from NYU and is pursuing a DNP at Villanova University. Liz has held positions in clinical practice, nursing professional development and nursing leadership at MSK. Throughout her career, Liz has been dedicated to the development nurses as leaders in the profession and community. Elizabeth is a member of ONS, Sigma Theta Tau, AONL, ANA, the School of Health Professions and Nursing Advisory Board at Long Island University, Chamberlain DNP Program Preceptor Advisory Board and is a mentor with The Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare. She received the ANPD Belinda E. Puetz award for excellence in professional development and the Samuel and May Rudin Award for Excellence in Nursing Education at MSK.
Aoyjai Montgomery, PhD, BSN; University of Alabama at Birmingham; Birmingham, Alabama
Dr. Montgomery received a BSN from Thamasart University, in Thailand. She worked as a pediatric nurse for Thamasart University Hospital in Thailand for 4 years and came to the U.S. to pursue her PhD. She received her PhD from School of Nursing, University of Alabama at Birmingham (UAB) in 2019 and was offered a post-doctoral fellow position at School of Nursing, UAB. Dr. Montgomerys studies focus on nurses burnout, well-being and health, work environment and patient safety and patient outcomes. Her work also involves how shift work, burnout, sleep, and circadian misalignment in nurses impacts patient and nurse safety. She is an expert on data analysis and interpretation, as well as data visualization. She is a statistical consultant for DNP and PhD projects as well as being a data analyst for numerous research projects and teams.
Kathleen Morales, PhD, RN, CNE; University of West Georgia; Rome, Georgia
Dr. Morales received her PhD from Georgia Baptist College of Nursing of Mercer University. Her dissertation research was a mixed methods, feasibility study which tested the effect of a resident-focused hand hygiene intervention in a long-term care facility. Dr. Morales has over 30 years experience as a Registered Nurse. Her practice areas include adult medical/surgical, orthopedics, emergency department, and intensive care. Dr. Morales is a contributor to five books: Legal Nurse Consulting: Principles & Practice; The Emergency Nursing Bible; NCLEX-RN Review. Keeping it Real! Simplified; Nursing Made Easy; and Pharmacology Made Easy. She is an associate professor at the University of West Georgia. . She is on Twitter @KMorales and on LinkedIn Katie Aumann Morales, PhD, RN, CNE
Courtney Mulder, BSN, RN, CEN; College of Nursing at The Ohio State University; Columbus, Ohio
Courtney Mulder, BSN, RN, CEN is a current doctoral student at the Ohio State University in Columbus, Ohio. She has over eight years of experience in trauma and emergency department settings ranging from level one trauma centers to critical access hospitals. She brings experience as a staff nurse, charge nurse, and other various clinical leadership roles. She credits her ability to tell a meaningful story from her fellow emergency department colleagues who are some of the best storytellers in healthcare.
Holly Muller, DNP, MHA, RN, NEA-BC, CRRN; UCF CON; Cape Coral, Florida
Holly Muller most recently served as the Chief Nursing Officer for Orlando Health Orlando Regional Medical Center and Assistant Vice President, Orlando Health. In May 2022, she will join Presbyterian Healthcare Services in Albuquerque, New Mexico, as the SVP, System Chief Nurse Executive. Holly is an accomplished executive nurse leader with a proven track record of delivering quality results, leading complex facility projects, and developing high-performing teams. Holly recently completed the Doctor of Nursing Practice program at the University of Central Florida. She completed the Wharton Executive Nurse Leaders Program and is board certified as a nurse executive. Holly serves on numerous boards and is an active member of healthcare and nursing organizations, participating in Sigma Theta Tau International since becoming a registered nurse. Holly is passionate about mentoring youth and has volunteered as a GED tutor with Lifeline Family Center and a student mentor with the Big Sisters Organization.
Toni Murray, DNP, CENP, NPD-BC, CMSRN; AMN Healthcare; Upper Marlboro, Maryland
Dr. Toni Murray has practiced as a nurse for over 27 years and served in Nursing Education & Professional Development for the past 15 years. Most recently, Toni served as the Director, Nursing Education & Professional Development for MedStar Southern Maryland Hospital Center. She is a Fellow of the University of Maryland Nurse Leader Institute and serves as Co-Founder and Secretary on the Board of Directors of DNPs of Color. Dr. Murray currently serves as Director, Clinical Education & Professional Practice for AMN Healthcare.
Heather Nelson-Brantley, PhD, RN, NEA-BC; University of Kansas; Kansas City, Kansas
Heather Nelson-Brantley, PhD, RN, NEA-BC, is an Assistant Professor and Leadership Program Director at the University of Kansas School of Nursing. Dr. Nelson-Brantley uses implementation science approaches to study organizational change, nursing practice environment, rural healthcare delivery, cancer, and palliative care. She is an alumna of the NIH and V.A. co-sponsored Training Institute for Dissemination and Implementation Research in Health. She has led and worked on several implementation science studies, including her current study to understand how to optimize patient-clinician communication through open notes in the diagnosis and treatment of cancer. Dr. Nelson-Brantley developed an innovative PhD-DNP collaborative learning course on implementation science. She is well published in nursing leadership science and implementation science. Her article, Using Implementation Science to Improve the Adoption and Implementation of Advance Care Planning in Rural Primary Care was recently recognized as a top-cited article in the Journal of Nursing Scholarship from 2020 2021.
Kama Newbry, RN-BC, BSN, PHN; UCLA Health; Los Angeles, California
Kama has been a nurse for 15 years, during which time she has spent her career blending her passion for patient care and her calling to improve the healthcare environment for caregivers. She has been an educator for the UCLA School of Nursing, taught nationally for a major med-tech company, and consults in the medical startup industry. After experiencing commonalities in each of the over 100 healthcare settings she has had the privilege to work with, she set her intentions to improve healthcare for everyone by implementing projects that have the potential to benefit nurses nationwide. Her vision is a healthcare system that empowers nurses to be at the forefront of system design by bringing the decisions made into the hands of those implementing and most impacted by said decisions.
Stephanie Nolan, DNP,MBA,RN,CPAN, NEA-BC; Providence Little Company of Mary; Los Angeles, California
Dr. Nolan is Executive Director of Nursing at Providence Little Company of Many in Los Angeles, California. .She oversees the clinical, operational and financial aspects for the Behavioral Health Service Line , the Acute Rehabilitation Center as well as the Acute Care nursing departments. She is recognized for developing leaders, inspiring innovative engaged teams and creating diverse, healthy work environments. Prior to joining Providence, Dr. Nolan served as the Director of Nursing for PeriAnesthesia Services at New York Presbyterian Weill Cornell Medical Center in New York, NY. Dr. Nolan earned a Masters in Nursing Administration (New York University), a Masters in Business Administration with a Healthcare Administration focus (Walden University), and received her DNP from Case Western Reserve University Dr. Nolan attended the Nursing Leaders Program at the Wharton School, University of Pennsylvania and carries national certifications as a Certified PeriAnesthesia Nurse (CPAN) and Board Certified Advanced Nurse Executive.
Dónal OMathúna, PhD; The Ohio State University; Columbus, Ohio
Dónal OMathúna is Associate Professor at The Ohio State Universitys College of Nursing and the Center for Bioethics. He conducts systematic reviews as Director of the OSU Cochrane Affiliate at the Fuld Institute for Evidence-based Practice. His research addresses ethics during disasters and humanitarian crises, including disaster research ethics and One Health ethics. He has been a PI on funded research in Europe and the US. He is a member of research teams investigating moral distress and moral injury during COVID-19. He has contributed to ethics initiatives with WHO and UNICEF, authored numerous peer-reviewed articles and co-edited several books.
Rebecca Owens, DNP, MBA, MSN, RN-BC; NYS Psychiatric Institute @ Columbia; New York, New York
Dr. Owens is Chief Nursing Officer, New York State Psychiatric Institute (NYSPI) overseeing development, implementation, and evaluation standards of nursing practice, clinical decision making, and quality of care monitoring. She is responsible for facilitation of evidence-based practice, recruiting and hiring procedures, and nursing department material/fiscal resource management, research, and education. Prior to joining NYSPI, Dr. Owens was the Patient Care Director and Interim Director of Nursing & Quality at New York-Presbyterian Hospitals Payne Whitney Manhattan Inpatient Psychiatric Unit, Comprehensive Psychiatric Emergency Program (CPEP), and Mobile Crisis Community Outreach Program. She holds a Doctor of Nursing Practice (DNP) from Case Western Reserve University, Masters in Nursing Science (MSN) from University of Phoenix, a Masters in Business Administration (MBA) - Marketing, and Strategic Planning from City University London, a BA from the George Washington University, and an Associate of Applied Science in Nursing (AAS) from Cochran School of Nursing.
Joy Parchment, PhD, RN, NEA-BC; University of Central Florida College of Nursing; Orlando, Florida
Joy Parchment, PhD, RN, NEA-BC currently serves as an adjunct professor for the University of Central Florida. She actively publishes about professional nursing practice, work environments, the nurse manager role, leadership competencies; diversity, equity, and belonging; and nursing leadership science strategic priorities. Dr. Parchment holds board certification as an advanced nurse executive from the American Nurses Credentialing Center (ANCC), a patient safety officer certificate from the Institute for Healthcare Improvement (IHI), a Fundamentals of Magnet certificate through ANCC, Leadership certification from Maxwell Leadership, and certification as a Virtual Presenter and Virtual Host through eSpeakers. She on the editorial board of Nursing Administration Quarterly, and a reviewer for numerous other scholarly nursing leadership journals.
Patricia Patrician, PhD, RN, FAAN; University of Alabama at Birmingham; Birmingham, Alabama
Dr. Patrician earned a BSN from Wilkes University, Wilkes-Barre, Pennsylvania; MSN in Critical Care from the University of Texas Health Science Center, San Antonio, Texas; and PhD in nursing from the University of Pennsylvania, Philadelphia, PA. She is a Fellow of the American Academy of Nursing. She joined the UAB faculty in 2008 after having served 26 years in the US Army Nurse Corps, where she held clinical, administrative, educational, and research positions. At UAB she teaches and mentors students in the PhD and the Executive DNP Programs. She conducts research on the nursing workforce and nursings contributions to patient safety and quality outcomes. Dr. Patrician is Co-Director of the VA Quality Scholars (VAQS) fellowship program at the Birmingham, AL site and mentors post-doctoral nurses, physicians, and pharmacists in quality improvement and improvement science activities. She has authored or co-authored over 70 peer-reviewed publications and several book chapters.
Grant Pignatiello, PhD, RN; Case Western Reserve University; Cleveland, Ohio
Dr. Grant Pignatiello is an Instructor and NCATS KL2 Scholar at Case Western Reserve Universitys Frances Payne Bolton School of Nursing. His research examines translational approaches to improving decision-making during critical illness. He has published and presented his work at regional, national, and international venues, and is nationally recognized as an emerging leader in his field.
Andy Pilarte; Brigham Young University; Provo, Utah
Andy Pilarte, Research Assistant, is currently an undergraduate nursing student in the Brigham Young University College of Nursing, Provo, Utah.
Anne Pohnert, MSN, BSN, FNP-BC, RN; CVS Health; Woonsocket,, Rhode Island
Anne Pohnert is an Advanced Practice Registered Nurse and has been board certified as a Family Nurse Practitioner for over 20 years. She currently serves as the Lead Director of Clinical Quality for MinuteClinic, a national convenient care organization with over 1,200 clinics in 35 states and the District of Columbia. Anne leads the national MinuteClinic Clinical Quality program, including clinical quality improvement initiatives, quality measurement, and quality dashboard development, Joint Commission Ambulatory Care Accreditation, the MinuteClinic infection prevention programs, clinical quality reviews and policies and procedures. As the Pathway to Excellence Program Coordinator, Anne played a key role in MinuteClinics successful designation as an ANCC Pathway to Excellence Organization in 2019. She is the Co-Principal Investigator on an Age-Friendly Health Systems Implementation Grant from The John A. Hartford Foundation, in collaboration with the Case Western Reserve University Frances Payne Bolton School of Nursing and the Institute for Healthcare Improvement.
Angela Prestia, PhD RN NE-BC; Trustbridge/ Florida Atlantic University; Tequesta, Florida
Dr. Prestia has been a nursing professional for over 40 years. She began her educational journey as an associates degree nurse, obtained a Bachelors in Nursing at the University of West Florida a Masters degree in Nursing from Vanderbilt University and a PhD is from Florida Atlantic University. She holds a Certificate in Health-care Administration and is board certified as a Nurse Executive. Her scholarship has led her to research, present and publish articles related to Nursing Leadership including; Chief Nursing Officer Sustainment, Nurse Executive Mental Health, Leadership Advocacy, Transformational Resiliency, and Moral Distress. Her hope is to share her results, passion and deep respect for all nurse leaders. She is a member in good standing of ALSN. She currently serves as President-Elect.
Vuong Prieto, PhD, RN, CHSE; UT Health Houston Cizik School of Nursing; Houston, Texas
Vuong Prieto is an Assistant Professor of Clinical Nursing for the Department of Undergraduate Studies at the UT Health Houston Cizik School of Nursing. She received her Bachelors of Science in Nursing at UT Health Science Center San Antonio, her Masters of Science in Nursing education at UTMB Galveston, and her Doctor of Philosophy in Nursing at UT Health Cizik School of Nursing. Her clinical background is mainly child and adolescent healthcare. She was a pediatric nurse for nine years and then transitioned to teaching baccalaureate-nursing students for over nine years. Her research interests include caregivers of children with medical complexity and simulation in undergraduate nursing education.
Marie Prothero, PhD, RN, FACHE; Brigham Young University College of Nursing - Provo, UT; Provo, Utah
Dr. Marie M. Prothero has over 30-years experience working in hospital and nurse executive roles focusing on developing teams related to patient safety, performance improvement, and hospital operations. Dr. Prothero is currently an assistant professor position in the College of Nursing, Brigham Young University. Dr. Prothero is a fellow in the American College of Healthcare Executives and serves on the Publication Committee for the American Organization of Nurse Leaders. She has a Ph.D. in nursing from the College of Nursing, University of Utah, and is a Jonas Nurse Leader Scholar. Her research area of focus is on leadership, organizational support, and learning in hospital settings
Stephanie Prtenjaca, MScN, BA, RN; London Health Sciences Centre; London, Ontario, Canada
Stephanie is a staff registered nurse working in the Critical Care Trauma Center at London Health Sciences Centre in London, Ontario, one of Canadas largest acute-care teaching hospitals. Stephanie is a graduate of Western Universitys Master of Science in Nursing program and has a strong interest in nursing leadership, new graduate nurse transition, and health promotion.
Mary T. Quinn Griffin, MSN, MEd, PhD, RN, CNE, FAAN, ANEF; Case Western University; Cleveland, Ohio
Dr. Mary T. Quinn Griffin is the Associate Dean for Global Affairs, and the May L. Wykle Endowed Professor at the Frances Payne Bolton School of Nursing, Case Western Reserve University. She is the Assistant Provost for Outcome Assessment and Accreditation at Case Western Reserve University. She is responsible for Global affairs in the school of nursing and collaborates with international partners facilitating faculty activities and student exchanges. Dr. Quinn Griffin teaches primarily in the Doctor of Nursing Practice program with a focus on nursing theory, research methods, and curricular design. She has chaired over 40 Doctoral committees and a member of over 90 doctoral committees. She has authored 39 book chapters and over 60 peer reviewed publications. Dr. Quinn Griffin’s areas of specialization include Global Affairs, Education, Executive Leadership, Emotional Intelligence, workforce issues, and climate change and health. She is leading the climate change and health initiatives in the school of nursing developing new research and education programs. She has a Master’s in Nursing Science and a PhD in Nursing from Case Western Reserve University. She has a Master’s degree in Education from Trinity College, University of Dublin, Ireland. She is a Fellow of the American Academy of Nursing and a Fellow of the National League for Nursing's Academy of Nursing Education. She is a certified nurse educator with the National League for Nursing. In 2019 she received the Elizabeth Russell Belford Award for Excellence in Education from Sigma Theta Tau, the international nursing honor society.
Maria Quirch, MSN, RN, OCN; UCLA Health; Los Angeles, California
Maria received her BSN from UCLA Nursing and began in the New Graduate Residency Program at UCLA Health, Solid Oncology in August 2013. Since that time, Maria has been involved in nursing professional governance at UCLA Health, is an active member of the Oncology Nursing Society, and has presented work on High-Touch Wipe-Down to reduce C. diff rates at various conferences and is published in Oncology Nursing News. Maria assumed her first formal leadership position in August 2018 as the Assistant Director of the UCLA Resource Team (float pool) and received her MSN from Western Governors University, previously having been a bedside clinician and permanent charge nurse, and is currently the Unit Director for 4SW, the Solid Oncology unit at UCLA Health.
Rhiannon Rasmussen, MSN, RN, CNL; University Hospital; San Antonio, Texas
Rhiannon Rasmussen, MSN, RN, CNL is currently the Assistant Director of Emergency and Trauma Services and has been with University Health since October 2013. Rhiannon began her career as a pediatric intensive care nurse. She became the nurse educator for both the Pediatric Congenital Cardiac Unit and the Pediatric Emergency Department in 2016. She is responsible for leading quality and process improvement activities related to patient safety, accreditation standards, regulatory requirements and quality improvement across the service line. Rhiannon earned her Bachelor of Nursing in December 2010 and her Master of Nursing in May 2017 from University of Texas Health Science Center San Antonio. She is a member of the American Association of Critical Care Nurses and Clinical Nurse Leader Association. She has multiple abstracts and poster presentations for national conferences and publications.
Rosanne Raso, DNP, RN, NEA-BC, FAAN, FAONL; NewYork-Presbyterian/Weill Cornell; NYC, New York
Rosanne Raso is currently the Chief Nursing Officer for the Magnet-designated NewYork-Presbyterians Weill Cornell campus, the #1 hospital in the New York metropolitan area and #7 in the country. Previously she was the Chief Integration Officer for NYU Langone-Brooklyn and prior to that the Nurse Executive at Lenox Hill Hospital. As an experienced nurse executive, Rosanne is a national leader in improving the practice environment for staff, enhancing patient safety, and advancing nurse leadership. She is the Editor-in-Chief of Nursing Management, the Journal of Excellence in Nursing Leadership, a trusted resource for frontline leaders. She was inducted into the American Academy of Nursing in November 2018. Dr. Raso is an adjunct assistant professor for both the New York University Rory Meyers College of Nursing and Case Western Reserve University Frances Payne Bolton School of Nursing.
Donna Roberson, PhD, FNP-BC; East Carolina University; Greenville, North Carolina
Dr. Roberson is a board-certified family nurse practitioner, certified dementia practitioner and certified Alzheimers Disease and Dementia Care Trainer and associate professor of nursing. She has research interests in healthy aging, support and education for professional and lay caregivers of those living with dementia and mentors research with undergraduate and doctoral students. Dr. Roberson holds several leadership positions including executive director of Program Evaluation for the ECU College of Nursing, Chair of Unit Assessment, Chair of Personnel and Chair of the Tenure and Promotion committee.
Linda Roussel , PhD, RN, CNL, NEA-BC, FAAN; University of Texas- Houston; Houston, Texas
Dr.Roussel is a professor at the Cizik School of Nursing at UTHealth in the Department of Graduate Studies in Houston Texas. Prior to this role, she was a professor at University of Alabama at Birmingham, where she served as the Doctor of Nursing Practice (DNP) program director. She was a tenured professor at University of South Alabama College of Nursing where she managed the Executive Leadership and Clinical Nurse Leader tracks. Additionally, she was also instrumental in working with a team to establish the first post-masters DNP program in Alabama. In addition to her academic career, Dr. Roussel also held nurse executive roles in acute and long-term healthcare systems. She also serves as a consultant in management and leadership and has published textbooks in the field. Dr. Roussel earned her PhD from University of Alabama at Birmingham School of Nursing. She is a Fellow in the American Academy of Nursing.
Pamela Russman-Chambers, DNS, MPH, MPP, BSN, RN, NPD-BC; Kennesaw, Georgia
Education: DNS, Nursing, Kennesaw State University, Kennesaw MPH, Health Management and Policy, University of Michigan, Ann Arbor MPP, Public Policy, University of Michigan, Ann Arbor BSN, Nursing, Kennesaw State University, Kennesaw BS, Anthropology-Zoology, University of Michigan, Ann Arbor Work Experience: Professional Nursing Program Manager, Northside Hospital Clinical Development Program Coordinator, Northside Hospital Patient Care QI Specialist, Northside Hospital Perinatal Nurse Educator, Northside Hospital Staff Nurse, Family Centered Care, Northside Hospital Research Coordinator, Nephrology, Emory University Research Associate, Cardiology, University of Michigan
Rowena Samonte, RN MSN CCRN CNL; VA NORTH TEXAS HEALTH CARE SYSTEM; DALLAS, Texas
1. Rowena Samonte Nurse Manager VA North Texas Healthcare System. She has been serving the Dallas VA since 2008, started as a frontline staff nurse in Critical are unit, transitions as a Clinical Nurse Leader then currently functioning as a Nurse Manager in an Acute care unit. She obtained her Clinical Nurse Leader Degree at university of San Francisco in 2015 and graduated RN Bachelors Degree in Nursing in 1993. She has worked as a critical care nurse for 23 years in different facilities in Dallas area. She has earned DFW Preceptor of the Year award in 2018 2. Uruaku Obasi is Lieutenant Commander(nurse officer) in the United States Public Health Service. She serves as an Assistant Nurse Manager as her current duty assignment with VA- North Texas Dallas Healthcare System. She obtained her bachelors degree in Integrative Biology from UC Berkeley. She pursued her BSN and MSN/MPH degree from Johns Hopkins University. (55)
Madeline Sampson, BSN; Brigham Young University College of Nursing - Provo, UT; Provo, Utah
Madysen graduated from Brigham Young University, College of Nursing in April 2022.
Anahit Sarin-Gulian, MSN, BSN, RNC-NIC, NE-BC; UCLA Mattel Childrens Hospital; Los Angeles, California
Anahit is a Nurse Leader at UCLA Mattel Childrens Hospital who has advanced the professional ladder from a new graduate nurse to unit director in the past 25 years at UCLA RR NICU. She has a Baccalaureate in Science of Nursing and Masters in Nursing Administration.
Ryan Schalles, MSN, RN; Texas Tech University Health Sciences Center; Mansfield, Texas
Mr. Ryan Schalles is Instructor at Texas Tech University Health Sciences Center in the Traditional Undergraduate Program. Ryan is a native of Lubbock Texas. He earned both his BSN and MSN from Texas Tech University Health Sciences School of Nursing. His background is in Emergency Nursing practicing at University Medical Center, the regions only level 1 trauma center. He returned to his alma mater in 2021 as a Faculty member at the Mansfield Campus in the Dallas-Fort Worth area.
Nathanial Schreiner, PhD, MBA, RN; Case Western Reserve University; Cleveland, Ohio
Dr. Nathanial Schreiner is an Assistant Professor at the Frances Payne Bolton School of Nursing, Case Western Reserve University and faculty member in the Marian K. Shaughnessy Nurse Leadership Academy. Dr. Schreiner has 22 years of clinical, administrative, and academic experience and is currently Lead Faculty for the MSN in Leadership and Administration at the Frances Payne Bolton School of Nursing. His program of research within nursing leadership science focuses on understanding the impact of leadership on nursing and patient-related outcomes.
Andrea Schuermann, MSN, RN, CNML; Orlando Health South Seminole Hospital; Longwood, Florida
Andrea Schuermann is the Manager for Quality Process Improvement & Patient Safety at Orlando Health. She has been with the organization since 2006, during her tenure she has held many positions from clinical nurse to nursing operations leader, professional practice, system improvement, and quality. Andreas undergraduate degree is from Lenoir-Rhyne University and her masters from the University of Cincinnati. She is currently in the PhD program at the University of Central Florida. She holds certification in nurse leadership from American Organization of Nurse Leaders (AONL). She is active in her professional organization, serving as adjunct faculty for the CNML Review Course and on the Annual Conference Planning Committee. She has led several system level process improvement projects and implementation of a system-wide patient acuity system. She is passionate about shaping the environment for clinical nurses to be successful and providing the tools and skills for nurse leaders to lead effectively.
Judith Shamian, RN, PhD, D.Sc, (Hon), LLD (Hon), FAAN, FCAN; Canada, Canada, Canada
Judith is the ICN President Emerita; past President of the Canadian Nurses Association (CNA); a professor of nursing at the University of Toronto; Professor at Case Western University, USA, Honorary Professor at Capital University, Beijing, China and established the Office of Nursing Policy at Health Canada. Dr. Shamian executive experiences span from, hospital, community, governments: national and international levels including policy and research. She is the recipient of numerous honorary Doctorates and awards including the Canadas Most Powerful Women: Top 100 award; the Golden Jubilee Medal from the Governor General of Canada; and the CNAs Centennial Award.
Todd Smith, PhD, MSHA, MBA, RN, NEA-BC; The University of Alabama; Tuscaloosa, Alabama
Dr. Smith is an Assistant Professor at the University of Alabamas Capstone College of Nursing (UAs CCN). He regularly teaches graduate courses related to leadership, healthcare management, health services delivery systems, and nursing administration. He has published and/or works on numerous research projects related to rural health care delivery systems, leadership, health care administration, health education, and telemedicine. In addition to earning his MSHA, MBA, and BSN, Dr. Smith holds a PhD in Health Services Administration, with a concentration in strategic management, from The University of Alabama at Birmingham (UAB), as well as Nurse Executive Advanced board certification. Prior to beginning his career at the University of Alabama, Dr. Smith worked as a health care administrator for more than 15 years, serving in a number of administrative leadership positions, mostly within UABs School of Medicine.
Todd B. Smith, MSHA, MBA, NEA-BC, RN; The University of Alabama; Tuscaloosa, Alabama
Dr. Smith is an Assistant Professor at the University of Alabamas Capstone College of Nursing (UAs CCN). He regularly teaches graduate courses related to leadership, healthcare management, health services delivery systems, and nursing administration. He has published and/or works on numerous research projects related to rural health care delivery systems, leadership, health care administration, health education, and telemedicine. In addition to earning his MSHA, MBA, and BSN, Dr. Smith holds a PhD in Health Services Administration, with a concentration in strategic management, from The University of Alabama at Birmingham (UAB), as well as Nurse Executive Advanced board certification. Prior to beginning his career at the University of Alabama, Dr. Smith worked as a health care administrator for more than 15 years, serving in a number of administrative leadership positions, mostly within UABs School of Medicine.
Madeline Sorhus, SN; Brigham Young University College of Nursing - Provo, UT; Provo, Utah
Maddie is a student nurse and research assistant at BYU. She will graduate in December 2023.
Rachel Stangland, MSN, RN, CNOR; Schneck Medical Center; Seymour, Indiana
Rachel Stangland is the Manager of Surgical Services, PCS Education, and the Magnet Program at Schneck Medical Center in Seymour, Indiana. Rachel has a Master of Science in Nursing and is a Certified Operating Room Nurse. She has more than 10 years of experience spanning professional practice, education, leadership, and project management. Resiliency is a key topic of interest in clinical practice, particularly in light of the global COVID-19 Pandemic. Rachel became interested in exploring this topic to improve staff morale, retention, and engagement.
Maya Stephenson; Brigham Young University; Provo, Utah
Maya Stephenson, Research Assistant, is currently an undergraduate nursing student in the Brigham Young University College of Nursing, Provo, Utah.
Patricia Stone, DNP, MSN, RN; Walden University; Minneapolis, Minnesota
Patricia Stone, DNP, MSN, RN Contributing Faculty Walden University Patricia.stone@mail.waldenu.edu Patricia Stone has been dedicated to the profession of nursing and quality patient care for more than 35 years. With a strong clinical background as an intensive care unit nurse and then in progressive leadership roles, serving as a Chief Nursing Officer for over sixteen years in both Level I Trauma and teaching hospitals, Patricia is known for consistently leading efforts to improve patient outcomes through evidence-based care. Recently, Patricia transitioned to the role of contributing faculty with the goal of mentoring future nurse leaders.
Kaleigh Sullivan, RN, BSN; University of Rochester; Rochester, New York
My name is Kaleigh Sullivan, I am currently a student in the University of Rochester's masters in nursing education program, and will be graduating this May. I am also a full time nurse in the affiliated medical center's inpatient child and adolescent psychiatric unit. During my time as a staff nurse, leader, and student I have found myself intrigued by the amount of compassion nurse's are capable of. This then brought me to how much nurses can suffer due to compassion fatigue and burnout. Through my research I am hopeful to bring this issue to the forefront of nurse leadership's attention, helping to both prevent and treat it.
Esther Thatcher, RN, PhD; University Hospitals; Cleveland, Ohio
Esther Thatcher RN, PhD is a Nurse Scientist in Population Health at University Hospitals. In this role, she develops multidisciplinary research and scholarly work to improve disease prevention and management services with a focus on health equity. Her current research focuses include early detection of chronic kidney disease, community approaches to cardiovascular health, and cancer screening. With a 20-year career as a registered nurse, Dr. Thatcher gained broad clinical experience in adult primary care, inpatient acute care, community health, and public health sector.
Sharon Tucker, PhD, APRN-CNS, PMHCNS-BC, NC-BC, FNAP, FAAN; The Ohio State University; Columbus, Ohio
Dr. Tucker studies, practices and teaches in the areas of behavioral interventions for mental health and wellness and implementation science to promote uptake of evidence into practice. She specifically focuses on women and children, employees and worksite interventions for health, well-being, resilience and mental health. She is certified as a mental health clinical nurse specialist, integrative nurse coach and meditation/mindfulness teacher. Dr. Tucker is a Robert Wood Johnson Executive Nurse Fellows Program Alumna; an elected fellow of the American Academy of Nursing (AAN) and National Academies of Practice; serves as Associate Editor for Worldviews on Evidence-Based Nursing; is President-elect for the Midwest Nursing Research Society; publishes widely and serves on regional and national boards.
Todd Tussing, DNP, RN, CENP, NEA-BC; College of Nursing at The Ohio State University; Columbus, Ohio
Todd E. Tussing, DNP, RN, CENP, NEA-BC is Assistant Professor of Clinical Nursing for the College of Nursing at The Ohio State University. He has over 34 years of nursing experience of which 30+ years have been in some type of leadership role. He has held the titles of nurse manager, director, and administrative director in urban/rural hospitals as well as an academic medical center. Dr. Tussing originally was a diploma nurse. Following his BSN, he obtained his MS and DNP from Wright State University. Dr. Tussing currently holds dual certifications in nursing administration. He has taught in an associate degree pre-licensure program, RN-BSN program, and a Master of Science program. He currently teaches in the Master of Healthcare Innovation program and DNP program at OSU College of Nursing. Courses he teaches include: Leadership, Health Policy, Quality Improvement, Best Practices in Organizational Operations, and Innovation in High Performing Organizations.
Todd E. Tussing, DNP, RN, CENP, NEA-BC; Ohio State University; Columbus, Ohio
Todd E. Tussing, DNP, RN, CENP, NEA-BC is Assistant Professor of Clinical Nursing for the College of Nursing at The Ohio State University. He has over 34 years of nursing experience of which 30+ years have been in some type of leadership role. He has held the titles of nurse manager, director, and administrative director in urban/rural hospitals as well as an academic medical center. Dr. Tussing originally was a diploma nurse. Following his BSN, he obtained his MS and DNP from Wright State University. Dr. Tussing currently holds dual certifications in nursing administration. He has taught in an associate degree pre-licensure program, RN-BSN program, and a Master of Science program. He currently teaches in the Master of Healthcare Innovation program and DNP program at OSU College of Nursing. Courses he teaches include: Leadership, Health Policy, Quality Improvement, Best Practices in Organizational Operations, and Innovation in High Performing Organizations.
Sonia Udod, RN,PhD; University of Manitoba; Winnipeg, Manitoba, Canada
Dr. Sonia Udod has an active program of research on healthcare leadership and expertise in qualitative research. As Co-PI for Creating and Translating Evidence for Nursing LEADership and Health Services (Lead Outcomes Research), my research program focuses on nurse leader development critical to supporting high-quality healthcare environments leading to quality nurse, patient, and organizational outcomes. I have been a Co-I on CIHR and Co-PI SSHRC, and PI on SHRF funded projects. Upon the invitation of Dr. Linda McGillis Hall, I serve with her as Co-Chair of the Leadership, Management and Policy in the Nursing Education Interest Group of the Canadian Association Schools of Nursing (CASN), and served as the International Director, Association of Leadership Science in Nursing.
Lynn Varagona, PhD, MSN, MBA, PMHCNS-BC, RN; Kennesaw State University; Atlanta, Georgia
Dr. Lynn Varagona is an Associate Professor of Nursing at Kennesaw State University, a Board Certified Psychiatric-Mental Health Clinical Nurse Specialist, and a licensed Psychologist. She holds a PhD in Community/Organizational Psychology from Georgia State University, an MBA with a concentration in the Business of Health Care from Emory University, a Master of Science in Nursing from the Yale University, and a Bachelor of Science in Nursing from the University of Florida. Dr. Varagonas research, which focuses on creating healthy practice environments through team virtuousness and team trust, has led to presentations at national and international conferences and publications in the Journal of Nursing Management, Nurse Educator, Nurse Education Today, SAGE Research Methods Medicine & Health Cases, Journal of Human Services, Journal of Faculty Development, and Journal of Allied Health.
Grace Vargas, RN, BSN, PCCN; UCLA Health; Los Angeles, California
Grace Vargas, brings 9 years of nursing experience to UCLA health. She started her career in Connecticut in medical oncology. She worked throughout the country as a travel nurse and returned to her passion in oncology at UCLA Health in 2015. Soon after beginning her journey with the organization, Grace became a charge and resource nurse, and grew to become a mentor and preceptor for many. Grace participated in our journey to Magnet by acting as an escort and scribe. She was a member of the professional and structure development councils, and took part in our community outreach group. In this role, she participated in events to feed and vaccinate the Los Angeles homeless community. Grace was promoted to assistant director for the Resource Float Team, managing over 200 CNAs, hiring and onboarding over 120 CNAs, and is currently enrolled in a Master of Science in a Nursing leadership program.
Javiera Villarroel; Brigham Young University; Provo, Utah
Javiera Villarroel, Research Assistant, is currently an undergraduate nursing student in the Brigham Young University College of Nursing, Provo, Utah.
Brandi Virgin, MSN, RN; UT Health Houston CSON; Houston, Texas
Brandi Virgin is an Instructor in Nursing at UT Health Houston CSON. She graduated with her BSN at Texas Woman's University and obtained her MSN in Nursing Education at UTH Health CSON. Her clinical background in nursing care of premature neonatal patients in Level III and IV NICU. Her teaching background includes pediatric nursing and pediatric nursing simulation in undergraduate nursing.
Joachim Voss; Case Western Reserve University; Cleveland, Ohio
Dr. Voss was added as first author. Please contact for bio information
Betsy Wagner, MSN, RN, CCRN-K, NEA-BC; The University of Kansas Health System; Kansas City, Kansas
Betsy Wagner is a nursing director for the acute care division since February 2019. She began her nursing career in 2004 all within The University of Kansas Health System. From a nursing assistant, bedside ICU nurse, nurse educator, education specialist and then the nurse manager role in 2012. An organizational goal of improving labor management is what sealed Betsys transition to managing the float pool and opening the resource management center in 2015. She received both her BSN and MSN in nursing informatics from the University of Kansas. Betsy is certified with both her CCRN-K and NEA-BC. Betsys desire to drive change and impact new nurse leaders is one of many reasons she loves working at TUKHS. When Betsy is not at work, she enjoys spending time in the outdoors with her family and Labradors.
Cathy Ward, PhD, RN, NEA-BC; University of Alabama at Birmingham; Birmingham, Alabama
Cathy Rodgers Ward is an Executive Scholar in Residence with the Executive Doctorate in Nursing Practice Program at the University of Alabama in Birmingham. She has over 30 years of executive management experience including Chief Nursing Officer at the UCLA Ronald Reagan Medical Center. Dr. Ward has a special interest in utilizing simulation to teach administrative concepts such as Executive Presence and Coaching Leadership. Most recently she was the Chief Nursing Officer for a quaternary academic medical center, UCLA Ronald Reagan Medical Center, ranked in the top three in the nation and, including a world-renowned childrens hospital, Mattel Childrens Hospital UCLA. Dr. Ward has a special interest in utilizing simulation to teach administrative concepts such as Executive Presence and Coaching Leadership.
Nora Warshawsky, PhD, RN, CNE, NEA-BC, FAAN; NEW Nurse Leader Solutions, PLLC; Corolla, North Carolina
Nora Warshawsky, PhD, RN, NEA-BC, CNE, FAAN recently transitioned from Professor and director of leading executive leadership DNP programs to creating her own independent consultant business. Dr. Warshawsky is a recognized expert in nursing leadership science and her cutting-edge research is informing nurse manager and leader practice. She was awarded the 2022 AONL Foundation Nurse Researcher of the Year in recognition of the impact of her research on nursing leadership practice. Dr. Warshawsky is co-leading the ALSN and AONL Foundation research task force to initiate an academic-practice research collaborative. She serves on the American Nurses Credentialing Centers Commission on Pathway to Excellence and as the Associate Editor of Nursing Administration Quarterly.
Carol Watson, PhD, RN,CENP, FAAN,; Iowa City, Iowa
Dr. Watson is an Adjunct Clinical Professor with years of leadership experience. In 2019 Dr. Watson was named as one of the American Organization of Nurse Executives (AONE) inaugural fellow. Although she is not currently teaching at the UI CON, Dr. Watson is very active in securing preceptors for students in the colleges Doctor of Nursing Practice Health Systems program (DNP-HS). She also serves as a member of the colleges Clinical Nurse Leader advisory committee.
Penni Watts, PhD, RN, CHSE-A, FSSH, FAAN; University of Alabama at Birmingham; Birmingham, Alabama
Dr. Penni Watts, PhD, RN, CHSE-A, FSSH, FAAN is the Director of Clinical Simulation for the Office of Interprofessional Curriculum and Associate Professor at the UAB School of Nursing in Birmingham AL. Her clinical expertise is in critical care and ER nursing. Dr. Watts has been in nursing education for over 20 years. She has expertise in designing IP experiences for curriculum integration and faculty development in IP education and simulation with an ongoing passion for teamwork training. She chairs the SSH CHSE-A Subcommittee and the INACSL Standards Committee and also serves as a site reviewer for SSH Accreditation.
Susan Weaver, PhD, RN, CRNI, NEA-BC; Hackensack Meridian Health; Neptune, New Jersey
Susan H. Weaver, PhD, RN, CRNI, NEA-BC, a nurse scientist at Hackensack Meridian Health Ann May Center for Nursing and the New Jersey Collaborating Center for Nursing, has more than 30 years of nursing leadership experience. Her program of research focuses on the nursing workforce, particularly administrative supervisors and clinical nurses who work the night shift, and improving outcomes. Dr. Weaver has recently completed a qualitative systematic review on the experiences and perceptions of nurses working night shift. Currently she is conducting research on the lived experience of nurses during the pandemic, and the management of infusion therapy in ICUs during the pandemic. Dr. Weaver is an active member of the ALSN research committee and the AONLF-ALSN Advisory Group.
Meghan Weese, PhD, RN, CPN, NEA-BC, NPD-BC; Akron Children's Hospital; Akron, Ohio
Dr. Meghan Weese is Director of Nursing Professional Development and Engagement and Magnet Program Director at Akron Childrens Hospital. She is certified in nursing leadership, professional development, and pediatrics. She received a Bachelor of Science in Nursing from Kent State University and a Master of Science in Nursing Administration and Doctorate of Philosophy in Nursing from The University of Akron. Her dissertation study, Relationships among Mentoring, Empowerment, and Organizational Commitment in Nurse Leaders, was awarded grant funding through Sigma Nursing Honors Society, Delta Omega chapter. She has been an active member of a research team studying mentoring since 2007 in roles as primary investigator, co-investigator, primary author, co-author, and national presenter. Honors for Dr. Weese include the Delta Omega Lillian DeYoung Research-Based Knowledge Translation Award, Akron Childrens Hospital Nursing Research Council Expert Research Award, and Ohio Organization for Nurse Executives Aspiring Nurse Leader 40 Under 40 Award.
Holly Wei, PhD, RN, CPN, NEA-BC, FAAN; University of Louisville School of Nursing; Louisville, Kentucky
Dr. Wei is a Professor and Assistant Dean for the PhD Program at the University of Louisville School of Nursing. Her research focuses on organizational culture, leadership development, clinician well-being, stress genomic biomarkers, and patient care quality. Dr. Wei has published over 50 peer-reviewed articles and delivered about 80 presentations globally. She serves on three journals editorial boards, as an Associate Editor for the International Journal for Human Caring, and the Board of Directors for the International Association of Human Caring. Dr. Wei has authored a leadership book, Visionary Leadership in Healthcare, and published the Convergent Care Theory and five nursing and interprofessional practice models.
Teresa D Welch, EdD, MSN, RN, NEA-BC; The University of Alabama; Tuscaloosa, Alabama
Dr Welch received a Doctor of Education in Instructional Leadership from the University of Alabama 2016. She worked thirty years as a critical care nurse specializing in adult ICU with twenty-two years management experience prior to joining Capstone College of Nursing 2016. As an innovative leader and change agent, Dr Welch championed the implementation of the health systems Rapid Response Team working with an interdisciplinary team to develop and implement the program but to also revamp the resuscitation team integrating evidence-based best practice standards into resuscitation processes to provide a comprehensive data driven program focused on continuous quality improvement. During her tenure Dr Welch managed construction of two 16 bed state-of-the-art intensive care units and implemented a Peripherally Inserted Central Line team, and Continuous Renal Replacement Therapy program. Dr Welch holds a Nurse Executive Advanced Board Certification, with extensive experience in operations management and team building, Dr Welchs research interests lie in leadership competency development.
Bobbi Wilson, BSN; Brigham Young University College of Nursing - Provo, UT; Provo, Utah
Bobbi graduated from Brigham Young University, College of Nursing in April 2022.
Theresa A. Wurmser, PhD, MPH, RN, NEA-BC; Hackensack Meridian Health; Neptune, New Jersey
Teri Wurmser, PhD, MPH, RN, NEA-BC has over 45 years of experience in nursing and health care. Dr. Wurmser currently serves as Vice President of Nursing Research, Grants and Academic Affairs, Hackensack Meridian Health, Ann May Center for Nursing and is the founding Dean of the Georgian Court-Hackensack Meridian Health School of Nursing. She has been the project director for multiple, successful HRSA Workforce and Nurse Education, Practice, and Retention Program grants and is an experienced leader, grant writer and researcher.
Carli Zegers, PhD, APRN, FNP-BC; University of Kansas; Kansas City, Kansas
Carli Zegers, PhD, APRN, FNP-BC, is an Assistant Professor at the University of Kansas School of Nursing, and a nurse practitioner in the Emergency Department at Truman Medical Center. Dr. Zegers obtained her PhD and FNP from the University of Nebraska Medical Center with an emphasis on health literacy, self-management strategies, and underserved populations. Previously, Dr. Zegers was the principal investigator of the KC HealthTracks grant through the Office of Minority Health focused on developing a pipeline program for high school students from underrepresented and underserved backgrounds into healthcare professions. Dr. Zegers serves on multiple national boards focusing on diversity, health policy, and health communication. She is an AAN and Jonas Foundation Policy Scholar and most recently, awarded the ANF and UnitedHealth Group Jeannine Rivet National Leadership Award. Dr. Zegers is committed to improving the health of underserved and diverse populations and communities through practice, research, health policy, and leadership.
Abstracts
Ordered by Abstract ID (listing first author only)
82-R. Implementation Sciences Dynamic Sustainability Framework: A Study to Evaluate Alignment with Doctor of Nursing Practice Curriculum and Projects
Jeannie Corey
11/5/2022, 10:45am - 11:45am, Breakout 22
Implementation science in nursing has been touted as an evolution of evidence-based practice in doctor of nursing practice (DNP) education as core to translational nursing. This is significant to nursing leadership, patient and organizational outcomes to further reduce the evidence to practice gap. Implementation is a required, key component of the DNP project, yet, implementation science frameworks are inconsistently taught in DNP programs and thus not often identified in DNP projects. Without intentional focus on implementation through the lens of translational nursing, projects may not receive the full support by organizational leaders and stakeholders. The challenges of intervention sustainment can be enhanced through integrating themes of adaptive, contextually sensitive ongoing improvement and a learning healthcare system framework. This case study provides an example of how the use of implementation theories and frameworks in two university settings guide curriculum and project management development. Specifically, the dynamic sustainability framework (DSF) will be described relating to DNP curriculum inclusion and quality improvement projects impact and sustainability. The DSF provides a conceptual perspective of continued learning and problem-solving, ongoing adaptation of interventions with a primary focus of fit between interventions and multi-level contexts. DSF also considers expectations for ongoing improvement as opposed to diminishing outcomes over time. Through this case study approach, implications for improvement, change, leadership, and project management will be explored and described.
72-R. The Effect of Authentic Leadership and New Graduate Support on New Graduate Nurses Job Satisfaction
Stephanie Prtenjaca
11/3/2022, 1:15pm - 2:15pm, Breakout 1
Canada, like many other developed countries, is facing a serious shortage of nurses due to a series of factors, including an aging population, aging nursing workforce, higher workloads, limited resources, and stressful working conditions, exacerbated by growing financial pressures. Consequently, the retention of the nursing workforce has become a pressing concern and an international priority. The purpose of this study was to test a theoretical model linking authentic leadership to new graduate nurses job satisfaction through its effect on new graduate support. This study was a secondary analysis of Time 1 baseline data collected in a two-wave national study of Canadian new graduate nurses, which used a non-experimental, predictive survey design. A convenience sample of 215 new graduate nurses with less than two years of experience, working in direct care, was obtained through the College of Nurses of Ontario. Following ethical approval, data were collected through mailed standardized questionnaires using the Dillman Total Design Methodology. Hayes PROCESS macro for SPSS was used to test the hypothesized simple mediation model. Overall, the model accounted for approximately 31% of the variance in Ontario new graduate nurses job satisfaction. Results demonstrated a direct positive and significant relationship between AL and NGN job satisfaction, AL and new graduate support, and new graduate support and NGN job satisfaction, as well as the indirect positive and significant relationship between AL and NGN job satisfaction, mediated by new graduate support. The findings of this study provide preliminary understanding of the mediating role of new graduate support in the relationship between nurse managers authentic leadership and job satisfaction in Ontario NGNs. These findings contribute to the limited body of knowledge on the role of nurse managers authentic leadership, new graduate support, and NGN job satisfaction and suggest that authentic nursing leaders may contribute to improved new graduate support and new graduate nurse job satisfaction. Findings of this study suggest there are promising outcomes when AL is integrated into the planning, recruitment, development, and evaluation of leaders. As AL can be learned through training, organizations are strongly encouraged to invest in formal leadership programs for leaders to improve their AL. Moreover, healthcare and educational organizations must collaborate on ways to ensure their NGNs are supported in the workplace during their transition from student to professional roles. The development and presence of authentic nurse managers, within healthcare and nursing, can have a positive influence on the work environments and the work attitudes of their followers, which in turn can contribute to the creation of a sustainable nursing workforce for the future.
69-ASP. Increasing Nurse Leaders Knowledge and Competency in Authentic Leadership
Patricia Stone
11/3/2022, 1:15pm - 2:15pm, Breakout 1
ABSTRACT: Research has demonstrated a positive correlation between authentic leadership and positive patient and organizational outcomes. Given that nurses can be educated in authentic leadership, providing nurse leaders with training opportunities will help them develop authentic leadership skills which will benefit patients and the organization. At the project site, there is little opportunity for leadership development among nurse leaders. Thus, the purpose of this academic-practice partnership was to determine if an educational intervention focused on authentic leadership would increase knowledge and awareness among nurse managers. Twenty-three nurse managers were invited to participate in an educational intervention, and 20 individuals participated for an 87% response rate. The mean pretest score for knowledge was 7.45 (SD = 1.76); the mean posttest score was 8.75 (SD = 1.29). Using a Wilcoxon signed rank test to estimate the data, there was a statistically significant difference in pretest and posttest scores (z = 3.14, p < 0.01), indicating an increase in knowledge. Participants were also asked to assess their awareness of authentic leadership using a Likert scale between 1 and 7, with 1 = No awareness at all and 7 = Full awareness. The mean pretest self-assessment score was 3.65 (SD = 1.50), and the mean posttest self-awareness score was 5.85 (SD = 1.09). Using a Wilcoxon signed rank test to estimate the data, there was a statistically significant difference in pretest awareness and posttest awareness (z = 3.78, p < 0.001), indicating an increase in awareness. Additionally, a 14-session experiential authentic leadership program is underway to enhance nurse leaders authentic leadership competencies. This project contributes to positive social change by improving leadership skills among nurse managers, which can lead to improved patient and organizational outcomes.
56-QI. Proactive Staffing at the University of Kansas
Betsy Wagner
11/5/2022, 9:30am - 10:30am, Breakout 19
A core value and organizational talent management goal of the University of Kansas Health System is proactive staffing. We seek to ensure we are good stewards of our patients and organization. COVID-19 disrupted our approach to managing our workforce, requiring new thinking on how to utilize our current staff, and how we could position other resources within our system and the community to ensure we stayed true to that core value of remaining proactive in a time of constant change. We conducted an evaluation of staff at our facilities, including areas where services were suspended, as well as professionals in non-patient roles. We assessed current skills profiles, pervious roles, current and prior licensures, and training we could provide to ensure the delivery of care was not disrupted. We determined we had the bench strength to aide our nurses by creating a new RN Support role. We identified current staff who were still licensed RNs but were not providing direct patient care. The new role allowed us to deploy help for patient care to lessen the burden of our bedside staff. For example, RNs from Pain Management, Infection Prevention, Quality and Safety, as well as Nurse Educators had the previous experience and expertise to assist in many ways. On an individual level we assessed what tasks they were comfortable/able to perform to assist the RNs on those units. Additionally, RNs from Ambulatory and Surgical Services, areas that had been closed, had the ability to help as well. An additional role created during this time was the Patient Companion. This new skill was established to help support 1:1 patient monitoring. Any current employee could be trained and could sign up for extra hours including students from the university who were desperate to serve our organization and community. As a medical background was not a prerequisite to sit with a patient, we were able to provide them with appropriate training to free up RN resources to focus on bedside care. For all of these roles, we were able to create a flex pool within our predictive scheduling tool and assign these individuals to the areas they were competent and needed most. Because of the flexibility of our staff, their comradery, and their willingness to support patient care, we were able to maintain fill rates of 80% and above throughout the pandemic. Additionally, team members who took on these additional roles many of whom had not worked bedside for years received first-hand exposure to what is happening on the front lines and have been able to apply a more in-depth systemness understanding to how they approach their roles in quality improvement, education, and other areas of the organization. Although the pandemic is finally subsiding, the impact it made on our staff and our ability to continue to meet patient demand remains. We, like all other healthcare organizations, are now looking at new innovative ways to recruit and retain staff.
13-R. Presence of Authentic Nurse Leadership during the Pandemic: Two National Studies
Rosanne Raso
11/3/2022, 2:30pm - 3:30pm, Breakout 4
There has been much attention to the challenges faced by nurse leaders during the pandemic. We studied clinical nurses and nurse leaders perceptions of the presence of authentic nurse leadership and its attributes in two national quantitative studies during the COVID-19 pandemic, one in the summer of 2020 and one in the fall of 2021, using the DAISY Foundation database to reach US participants. There were more than 5000 nurses in the first sample and more than 1700 in the second study. Overall, we found the presence of ANL most of the time in both studies and all subscales were present as well. Self-awareness ranked highest and shared decision-making ranked lowest in both studies, although >3.0 and present most of the time. The manager/director subsets in both studies perceived higher levels of ANL from their immediate supervisor, 3.37 and 3.33 respectively. There was a moderate positive correlation of ANL to healthy work environment in both studies, replicated for the third time by this research team. Evidence for ANL as an effective leadership style is growing, even during these challenging times. The presence of ANL for these thousands of US nurses in both years of the pandemic (2020 and 2021) signals strong nursing leadership for our frontline nursing workforce. Authentic leadership is an essential standard for a healthy work environment which is critical moving forward to restore the environment for practice and retain/recruit our workforce after the disruptive pandemic acute care nursing exodus. ANL is a relational leadership style, and there are implications for nurse leader development as we move forward, aligned with identified needs for the future direction of nursing administration leadership science.
51-R. Women's Power in the Nursing Workplace: A Critical Qualitative Study
Kaitlyn George
11/5/2022, 10:45am - 11:45am, Breakout 22
In nursing, power is the ability to mobilize resources, produce intended effects, and actively take steps to empower patients. Empowered nurses are vital to creating a sustainable nursing workforce, providing high-quality patient care, and improving organizational outcomes. Nurse leaders play a vital role in empowering nurses. Despite the numerous benefits of empowered nurses, evidence suggests women working in healthcare are not adequately empowered. Lack of empowerment, in part, stems from the traditional hierarchy and power-based nurse-physician relationship, as well as societal gender biases and norms that are perpetuated within the hierarchical structure of healthcare systems. These inequities prevent female nurses from using their power in the workplace. Nurse leaders need to address these inequities to ensure nurses on their teams are fully empowered. Previous research provides insight into levels of nurse empowerment within the constraints of current systems and structures in healthcare. However, those studies reveal little about the factors associated with nurse empowerment. Additionally, they fail to question and challenge systems and structures that negatively impact womens ability to use their power in the nursing workplace. Nurse leaders must understand and address systemic barriers to womens power to improve staff, clinical, and organizational outcomes. Aim: The purpose of this study is to understand the factors that influence nurse empowerment and reveal structural barriers that prevent women from having power in the nursing workforce. We anticipate the insights gained through this study will guide nurse leaders efforts to resolve such barriers and empower the nurses on their teams. Methods: This study used a critical qualitative research design. Semi-structured interviews were conducted with 17 registered nurses working within in-patient hospital settings in Utah and New Mexico. Interviews were analyzed using thematic analysis. To improve rigor, we triangulated multiple interviews from multiple participants to inform our perspective about power structures, performed member checking, and conducted a thorough review of the literature to generate and test alternative explanations for our findings. We developed and used a coding system to ensure consistency between the coders. We also followed a detailed research protocol, maintained a database of all evidence generated through the study, and created chains of evidence to show the linkage between our findings, data, and research questions. Results & Implications: Six themes emerged from the data, four of which related to nurses power at work, and two which specifically related to how gender affects a nurses ability to use power and feel empowered. These themes were: (1) Supportive Leaders, (2) Positive Unit Culture, (3) Successful Advocacy, (4) Personal factors, (5) Societal Gender Roles, and (6) Sexism. Nurse leaders should strive to be supportive of their nurses and build a positive work environment while also providing consistent consequences when staff commit sexist actions. Nurses should take opportunities to advocate for their patients, exercise autonomy, and build their knowledge base to improve empowerment. Empowered nurses can revolutionize healthcare. The themes developed in this study will help nurse leaders and nurses alike increase nurses' ability to use their power and feel empowered in the workplace.
62-QI. Safe in the Storm or Making Waves? Safe Harbor & High-Stakes Communication
Delia Abbott
11/5/2022, 9:30am - 10:30am, Breakout 19
Context: A just and safe culture supports nurses who invoke Safe Harbor Nursing Peer Review when bringing patient safety concerns to their nurse leader. However, direct care nurses may fear bullying and retaliation by their nurse leader when invoking Safe Harbor. Nurse leaders may respond more effectively with a better understanding of Safe Harbor law. Aim: This innovation and evaluation project aimed to improve nurse leaders' verbal communication skills during a simulated high-stakes conversation and to increase knowledge of the Texas Safe Harbor Nursing Peer Review law. Methods: Nurse manager participants used an artificial intelligence-powered coaching platform to respond to two video simulations of a nurse invoking Safe Harbor. An education intervention was provided between pre-and post-assessment surveys. Results: Data show participants improved their confidence and competence in facilitating a high-stakes conversation and improved their knowledge of the Texas Safe Harbor Nursing Peer Review law. Conclusion: Effective communication is the foundation of nurse manager competencies and is vital to ensuring a just culture where nurses are empowered to raise safety concerns that impact patient outcomes. Keywords: Safe Harbor, nursing peer review, just culture, effective communication, nurse manager
37-R. Nurses Experiences with Change from Nurse-Patient Ratios to Workload Intensity Staffing
Cynthia Bacon
11/4/2022, 10:45am - 11:45am, Breakout 10
Aim: Exploring nurses' attitudes and perceptions regarding the change from nurse-patient ratios to workload intensity staffing, and the facilitators and barriers in implementing a workload intensity (WI) tool. Background: A WI tool was developed to quantify patient needs via workload points. The workload intensity staffing system was implemented to better meet patient needs and more equitably disperse nurses workloads. Methods: This was a qualitative, descriptive phenomenology study. Sixteen interviews were conducted with nurses from five adult inpatient units in one southeastern hospital in the United States. Questions focused on the nurses experience of the change to workload intensity staffing (WIS) and factors that helped or hindered the change transition. Results: Workload Intensity was perceived as a positive change. Final analysis revealed six themes related to the change to WIS: experiencing the change; balancing nurses' workload; standard work; challenges of the change process; workload intensity tool effective; and influences on change. Five themes were uncovered as facilitators and barriers to the change: resistance to change; intense workloads; supportive organizational culture; resources/training and evaluation. Conclusions: Allowing time for change adjustment and making the change resulted in balanced workloads with quantifiable data to justify staff assignments and verify increased workloads to leaders. Understanding barriers and facilitators to change are important for successful implementation of WIS. To promote success, leaders should provide support to staff and ensure availability of adequate resources. Implications for Nursing Management: Perceived lack of supervision and inconsistent use of the tool, both challenges to the change process, need to be addressed to ensure long-term success of the change.
33-R. Nursing Staffs Role in Detecting Urinary Tract Infections in Nursing Homes: An Integrative Review
Kimberly Delgado
11/4/2022, 10:45am - 11:45am, Breakout 10
Annually, 50-70% of nursing home (NH) residents are administered at least one antibiotic. Despite evidence-based protocols, of the antibiotics prescribed, 75% were prescribed inappropriately, and 50% were the wrong drug, dose, or duration with urinary tract infection (UTI) being the most common indication. In NHs, nursing staff spend a significant amount of time with the residents and are usually the first to recognize a change in condition. The purpose of this integrative review was to examine the state of the science to determine NH nursing staffs impact on the prescriptive process related to the identification and report of signs and symptoms indicative of UTI. This integrative review was conducted following Whittemore and Knafls recommended methodology. Level of evidence and quality were analyzed using Johns Hopkins nursing evidence-based practice guidelines. We used an a priori process to analyze non-experimental and experimental data and enhance rigor while reducing bias. In this review of 19 articles published between 2011 and 2020, three common themes were identified using constant comparative analysis: elements of antibiotic stewardship in NHs, nursings influence on prescriptive decision-making, and nursing staffs antibiotic stewardship responsibilities. In addition, while the prescriber was recognized as an expert in UTI management, the nursing staff in NHs were the individuals who recognized changes and communicated the residents needs to the prescribers. Further research must clarify the nursing staffs role(s) in detecting UTIs and their decision-making before reporting changes to the prescriber. Using this study as a foundation, future studies which include LPNs and CNAs may have a notable impact on NH regulations, education, and nursing scope and standards of practice. Keywords: nurse, nursing, licensed practical nurse, licensed vocational nurse, detection, urinary tract infection, long-term care, nursing home
11-ASP. A Post-Doctoral Program: Enhancing Academic Practice Partnerships
Linda Everett
11/5/2022, 12:00pm - 1:00pm, Breakout 25
There has been much attention to the challenges in enhancing academic practice partnerships. Many nurses prepared at the doctoral level, including those working in both academia and in healthcare delivery, have identified the need for additional mentoring and leadership development to advance their careers and assist them in navigating academic practice partnerships. Specific aims: Launch a post-doctoral program for academic and service leaders to address challenges for nurse leaders; contribute to the scholarly literature relevant to nursing literature and challenges in academic service partnerships; mentor nurse leaders in their professional career development. Process/procedures: We received significant support from the Samuel H. and Maria Miller Foundation to launch cohort #1 in June 2020. Due to the pandemic our plan to originally have an in-person program quickly switched to a virtual program. Each of the 11 participants was named a Miller Fellow. The 6 credit program was offered over 3 semesters with a 500 hour practicum in the final semester as the culminating experience for the post-doctoral program. Based on their background and their career goals, Fellows were paired with preceptors for the practicum experience. The practicum advisors included; Dr. Judith Shamian; Dr. Marian Nowak; Ms. Annette Kennedy; and Dr. Sharon Pappas. Outcomes: Each of the Fellows was expected to produce a scholarly paper as a result of the post-doctoral program. Topics of these published papers include: Resiliency Training for Italian Nurses; Black Minority Journey to Executive Leadership; Nurses and Telehealth: and Collaboration Between Public Safety and Quality Nurse Practitioner Education in Canada; and Reflections from a System Chief Nursing Executive: Intention to Lead. In addition, several Miller fellows contributed chapters to a new leadership and management text book to be published in 2022. This textbook will be used for graduate nursing education courses. Within the text there is significant attention to the values of academic practice partnerships for advancing the profession through stellar nurse leadership. Three of the Miller Fellows received new and expanded positions during this period. Michelle Acorn, DNP, NP PHC/Adult, FCAN was appointed Inaugural Chief Nurse for the International Council of Nursing, Geneva, Switzerland; Benjamin Farber, DNP, RN, CNL, NEA-BC, CENP became the Vice-President, Patient Care and Chief Nursing Officer at Eisenhower Health in Rancho Mirage, California; Kari Gali, DNP, APRN accepted the position of Director of Telehealth at Huron Consulting Group in Chagrin Falls, Ohio. Implications: Doctoral education alone is not sufficient; nurse leaders at all levels need to have access to formal educational opportunities to further develop their talents and skills in leadership. Formal post-doctoral programs with access to global speakers provide one avenue to advance nursing and nurses. Learning objectives: 1. Describe the post-doctoral program for nurse leaders with particular emphasis on the academic practice partnership components 2. Identify outcomes of cohort 1 completed in 2021 and implications for future cohorts.
68-ASP. Perspectives from Nurse Executives: Understanding Leadership Presence
Lyn S. Losty
11/5/2022, 12:00pm - 1:00pm, Breakout 25
Given todays healthcare environment, most healthcare organizations are facing tremendous pressures as disruption is becoming the new norm as many aspects of traditional care delivery are abruptly changing (Bleich et al., 2020). For example, this held true throughout the COVID-19 pandemic as it created stressful situations for organizations, patients, families, and providers, and especially nurses. While similarities exist across organizations in response to crises, there are differences in the environment in which crises occur and the way leaders respond to crises that create different platforms for how organizations and individuals respond and adapt to situations. For example, Burrell and colleagues (2009) hypothesized that given the logistics of catastrophic events, leadership skills remain of utmost importance. Thus, it is important to understand and explore current challenges of crises on health care delivery and leadership styles of nurse executives and apply these concepts to other situations to learn from our experiences. In a recent study, Losty and Bailey (2020) conducted a qualitative study in order to identify important concepts that described nurse leaders experiences during a crisis situation. One of the identified themes of the study was the concept of leadership presence as a quality important for nurse leaders. The purpose of this presentation is to: 1. Describe the concept of leadership presence and its relationship to nursing leadership. 2. Evaluate the concept of leadership presence in terms of professional nursing practice case study. 3. Formulate strategies that would assist in the improvement of patient and organizational outcomes.
47-QI. Developing Collective Mindfulness Skills in Nurse Leaders to Influence a Culture of Safety
Holly Muller
11/4/2022, 9:30am - 10:30am, Breakout 7
Core role accountabilities of nurse leaders are to create an environment that ensures quality, safety, and performance excellence. Although evidence supports health care systems' full engagement in high reliability organizing through collective mindfulness practices and behaviors, nurse leaders are often inadequately prepared to advance safety culture. Local metrics (2019-2020) demonstrated a need for safety culture improvement: 1) low scores in the AHRQ patient survey sub-section for supervisor, manager, or clinical leaders' support for patient safety, 2) hospital-acquired infections, pressure injury, and medication errors failed to meet internal benchmarks, and 3) only one-third of units met 95% compliance with regulatory documentation standards. Collective mindfulness, a cognitive process used to increase awareness and discriminatory details to discover and correct errors, is associated with lower turnover rates, and improved quality and safety. It increases both individual and team abilities to quickly assess complex systems and identify alternative actions, thereby reducing patient harm risk. By focusing on collective mindfulness and high-reliability organizing principles, a 20-bed critical care unit achieved a 60% improvement in reliability for the process measure of discharging patients alive with stable vital signs, resulting in a savings of $100/patient/day. Level III B evidence supports this quality improvement project. This project aimed to demonstrate that formal training in collective mindfulness skills for nurse leaders influences their leadership effectiveness in advancing safety culture, as measured by the Safety Organizing Scale (SOS). The objective was to implement a structured leadership development workshop on developing collective mindfulness skills in nurse leaders and evaluate the intervention's effectiveness. Thirty nurse managers participated in a 10-week interactive, educational workshop to develop and apply collective mindfulness skills using high-reliability organizing principles. The SOS tool provided measurement of safety culture and insight into the collective mindfulness practices among nurse leaders. The Framework for Safe, Reliable, and Effective Care (IHI) provided a roadmap for organizing the project design and developing nurse leaders to practice collective mindfulness as a critical process for advancing safety culture. The Plan-Do-Study-Act model for continuous quality improvement supported project implementation and aligned with the IHI's method for leading quality improvement. Measured by the SOS tool, twenty-one nurse managers' capability to influence safety culture with formal collective mindfulness training improved over three time points, baseline (50.04), mid-point (54.52), and end-point (58.86) by one-way ANOVA, p<0.001. Common themes from 81 narrative entries (n=19) included: 1) heightened awareness of the impact of nursing leadership on safety culture and outcomes, 2) proactivity versus reactivity for addressing safety concerns, and 3) the interactive workshop favorably impacted the learning process. The results support a positive association between collective mindfulness practices and nurse leaders' influence on safety culture. The interactive workshop model provided the time investment necessary to engage leaders in developing their capabilities for advancing safety within complex environments. We learned that the in-person workshop method contributed to team building in addition to application of content. Healthcare organizations should develop nurse leaders' collective mindfulness skills and embrace practices and policies that optimize safety culture.
53-R. Nurse Leader Attitudes and Beliefs on Medical Errors: Supporting Nurses Following a Serious Error
Marie Prothero
11/4/2022, 9:30am - 10:30am, Breakout 7
Problem/Background: Little is known about nurse leader attitudes, beliefs, training concerning medical errors, and how they perceive the recovery process for the nurses involved in such errors. Nurse leaders play a vital role in establishing the nursing culture. Although some institutions have shifted to a culture of safety and transparency to take the blame away from the individual involved in medical errors, it can be difficult for nurses to overcome the shame and blame they feel when they make a mistake. Nurses who feel supported by a nurse leader were able to stay working. When support was lacking, nurses left the department for employment elsewhere. Understanding nurse leader attitudes, beliefs, and training may help us understand these counterproductive reactions and help nurse leaders develop more effective approaches to addressing errors. Research Aim: This study identified nurse leader attitudes and beliefs on medical errors, training, and education provided or lack of training, and perceptions of how to help nurses recover from serious medical errors. Methods: A cross-sectional mixed-method (quantitative and qualitative) study was conducted with a convenience sample of nurse leaders in a designated leader role. An invitation to participate in this study was posted on the American Organization Nurse Leader website (AONL), e-newsletter, and community discussion board. Social media, Facebook, Twitter, and LinkedIn, were used to recruit additional participants. Participants consented to the study electronically and completed an electronic Qualtrics survey. Research Instruments: The Medical Error Attitude Scale (MEAS) survey elicited attitudes and beliefs on medical errors. The research team developed open-ended questions to explore nurse leader perceptions on education, training, and processes to mitigate the psychological sequelae of the error for the nurse involved. A demographic questionnaire gathered data about the type of nurse leader, years of experience, education level, experience with medical errors, age, sex, ethnicity, and current work setting. Data Analysis: Descriptive statistics will be completed using IBM SPSS v27 software. The MEAS is analyzed in three subscales, perception, approach, and causes of medical errors. Two items (10th and 13th items) are scored inversely. The total score is calculated by dividing the total score by the number of items in the measure. Scores below 3 are considered negative, and scores 3 and above are considered positive. Demographic data will be analyzed to describe the sample characteristics (percentages, range, and mean). Qualitative data from the open-ended questions will be analyzed and coded by categories and themes. Results: Results are pending. We anticipate discovering nurse leader attitudes and beliefs on medical errors and learning how nurse leaders support nurses following an error and best practices for intuitions to follow. We also anticipate learning more about the education and training nurse leaders receive on mitigating the nurse's emotional sequelae following an error. Implications: We anticipate the insights gained through this study will guide nurse leader efforts in education, training, and processes in supporting nurses following errors. This study is a starting point for providing resources to nurse leaders to fulfill their role to improve nurse well-being and improve patient care.
35-R. The Implementation of a Neonatal Multiple Patient Simulation in an Undergraduate Nursing Program
Vuong Prieto
11/4/2022, 2pm - 2:30pm, Poster
Background and Significance High-fidelity simulation is an effective teaching strategy that allows students to transfer what they learn in the simulation setting to the clinical setting (Carey et al., 2021). Nursing students have reported anxiety before neonatal intensive care unit (NICU) clinicals (Rashwan et al., 2021; Sim et al., 2021) due to patient fragility and higher risk for neonatal complications (Hockenberry et al., 2019). The current nursing education studies on multiple patient simulation (MPS) education report beneficial learning experiences (Davies et al., 2021). Specifically, students found MPS helpful for improving their communication and critical thinking skills (Horsley et al., 2014), patient safety competencies (Ironside et al., 2009), satisfaction with learning (Chunta et al., 2013), patient care prioritization and decision-making skills (Kaplan, 2010; Sullivan et al., 2019). Aim and Research Questions This study aims to fill a gap in existing research on the use of MPS for neonatal population in undergraduate nursing. Specific research questions are: 1. What are the changes in students reported anxiety levels before and after participating in a neonatal MPS experience? 2. What are students perceptions of the effectiveness of the neonatal MPS experience for meeting their learning needs? Study Design This is a descriptive, cross sectional pilot study. The target population is undergraduate nursing students. The sample will include 10-15 bachelors nursing students enrolled in the pediatric capstone clinical at UT Health Houston Cizik School of Nursing. The principal investigator (PI) is a faculty at Cizik and has access to students and the study setting, but is not responsible for grading the students who participate in the study. Permission and approval from the UT Institutional Review Board (IRB), Committee for the Protection of Human Subjects (CPHS) will be requested to conduct the study. Methods, Tools, Procedures All students will be included in one neonatal MPS in unfolding case scenarios to be developed by the researchers (See Appendix A). After the MPS, students will be asked by the PI to voluntarily participate in completing an emailed anonymous Qualtrics survey that will include questions about their demographics, and two validated tools - the State - Trait Anxiety Inventory (STAI) (Spielberger et al., 1983) and the Simulation Effectiveness Tool - Modified (SET-M) (Leighton et al., 2015) (See Appendixes B D). Data collection for the STAI will be a retrospective pre-post design. Faculty will use the Lasater rubric (Lasater, 2007) (See Appendix E) to evaluate student performance during the MPS. There are no risks to participation. Computers used to store data will be username and password protected with firewall and anti-virus protection. Analysis Descriptive statistics will be used to compare pre and post STAI scores (RQ1). Demographic data and SET-M scores will also be described (RQ2). Implications for Nursing Education This pilot study will contribute data on feasibility of neonatal MPS. The data will inform future studies and facilitate better transition to neonatal nursing practice.
73-EBP. Supporting Interim Nurse Manager Role Transition: The Development of an Evidence-Based Toolkit
Sandra Galura
11/3/2022, 4:50pm - 5:20pm, Poster
Interim nurse manages are frequently required during periods of transition, crisis, or change within an organization. The increasing financial pressures and clinical challenges faced by today's healthcare organizations has resulted in the need for interim nurse managers to fill nurse manager vacancies until permanent replacements can be found. With an average reported tenure for interim nurse managers (IMs) of up to 10 months, strategies to support IM role transition are lacking with 22% of IMs reporting no preparation for their role. The purpose of this evidence-based practice project is to identify strategies to support the role transition and professional development of interim nurse managers. The Johns Hopkins Nursing Evidence Based Practice Model will guide the development of evidence-based strategies to support IM role transition. The AHRQ Knowledge Transfer Framework along with feedback from nurse practice leaders and nurse researchers will be used to facilitate the transfer of research to practice. Findings from this evidence-based practice project will be used to guide the development of a package of tools to support interim nurse managers as they transition into and out of interim leadership roles.
55-QI. Decreasing Delirium with Prevention Interventions in the Intensive Care Unit
Heidi Karle
11/3/2022, 4:50pm - 5:20pm, Poster
Decreasing Delirium with Prevention Interventions in the Intensive Care Unit Heidi Karle, BSN, RN DNP Project Chair: Dr. Lindsay Davis, DNP, APRN-CNP DNP Project Team: Ann Alvarado, BSN, RN, Raeanne Fondriest, MS, APRN, AGACNP, Emilee Bird, MS, APRN-ANCS-BC Abstract Purpose: The purpose of this project is to determine if re-education of key delirium prevention interventions that are already in place, yet not routinely utilized, for bedside critical care nurses will decrease delirium in critical care admitted patients aged 18 years and older. Background/Review of literature: Delirium can occur in up to 87% of patients in the intensive care unit (ICU) (Kotfis et al., 2018). Delirium can lead to many consequences for the patient including increased length of stay, increased mortality risk, and increased risk of further complications. It is imperative that nursing professionals who are at the patients bedside perform a delirium assessment often to recognize delirium as soon as possible. Delirium is not a condition that is easily treated; therefore, multiple interventions should be put into place to try and prevent and/or decrease delirium in ICU patients (Mart et al., 2020). Key interventions such as appropriate lighting, early mobility, minimal sedation, and minimal ventilator days are suggested to aid in decreasing ICU delirium. Methods: An assessment of utilization of having lights on and blinds up in that patients room at appropriate times was performed both pre- and post-education with an assessment tool created by the project team, education on delirium, delirium interventions, and how to perform a Confusion Assessment Method for ICU (CAM-ICU) assessment was given to critical care bedside nursing staff, and CAM-ICU scores were assessed both prior to and after education as well as compliance with the key interventions stated above, following education. Implications for practice: Critical care nurses will be able to determine which patients are the most at risk for developing delirium, be able to accurately assess all intensive care patients for delirium and be able to implement important key interventions to decrease a patients risk of developing delirium. Keywords: delirium, ICU, CAM-ICU, assessment
57-EBP. Creating New Solutions for New Challenges in Nursing Leadership Through Leadership Residency Programs and Mentorships.
Todd Smith
11/3/2022, 4:50pm - 5:20pm, Poster
As the largest workforce within hospitals, nursing leaders stand to have a significant impact on quality outcomes and resource utilization. CMS directed reimbursement models such as value-based purchasing and pay-for-performance are focused on quality improvement and nursing excellence and are driving the financial landscape of healthcare delivery today. As a result, the quality and safety of patient care, patient outcomes, and the patient experience, along with the associated costs of providing that care are under intense scrutiny. Nursing leadership, particularly front-line managers, are strategically and uniquely positioned to have a significant impact in controlling the costs of healthcare while ensuring the quality of patient care and meeting operational demands with thin margins. Nurse managers self-perception of leadership competencies are influenced more by professional development and leadership competency training rather than professional experience or time served in a management role. According to AONE (2015), to be successful in a leadership role, nurse managers must demonstrate competence in all three domains of the Nurse Manager Leadership Domain Framework [NMLDF]: a) the Science: Managing the Business, b) Art: Leading the People, and c) Leader Within: Creating the Leader in Yourself. Demonstrating competence in all three domains will improve outcomes for the organization. As the complexities and demands of the healthcare environment have continued to evolve and escalate the need for leadership training, preparation, and transitional support have become a pre-requisite for successful leadership. To support new and emerging leaders in their transition to leadership roles we are proposing an evidence-based nurse leadership residency program focused on transition to leadership. As new graduate nurse residency programs are focused on the new graduates transition to professional nursing practice, so to the nurse leadership residency programs will focus on the leadership transition. As new graduate nurse residency programs have been proven to decrease nurse turnover rates within the first year, improve decision-making skills, improve morale, leadership skills and patient outcomes (AACN, 2015) so will nurse leader residency programs for nursing leadership. According to the literature, key drivers of manager job satisfaction are organizational support, mentorships, the quality of training and leadership competency development. Structured on-boarding processes improve management self-confidence, performance, and retention rates in front-line managers. Investing in your leadership team will have a sweeping and pervasive impact on the organization. From finance to quality metrics, to staff morale and stability and patient outcomes. As middle and upper management in organizations you have the training and the resources to effect organizational change.
63-QI. Keeping "U:" A-Float: Utilizing Information Technology to Disseminate Unit-Specific Practices that Support Float Team Staff Satisfaction
Adam Fronczek
11/3/2022, 4:50pm - 5:20pm, Poster
UCLA Health combined its Academic Medical Center and Community Hospital's Float Teams to align with the organization's vision of unity. The merged team employs approximately 865 RNs and CNAs who fill various staffing shortages in over 50 uniquely specialized units. The larger team brought on new challenges for float leadership as most of the staff are per diem. Their sporadic schedules do not allow for continuity of care or familiarization with unit-specific practices outside system-wide policies and standards. However, each unit is uniquely specialized and has precise needs for its respective patient populations. Therefore, the team needed a way to quickly access unit-specific details that supports the constant evolution of patient care. Evidence-based studies show float staff has overwhelming feelings of dissatisfaction, stress, and anxiety due to unfamiliarity of new patient populations, unit-based staff, and processes needed to succeed in each patient population. To enhance staff preparedness and reduce floating anxiety, the Keeping "U" A-Float project was developed to support the team's knowledge needed to provide high-quality care. Readily available tip sheets were created, which contained unit-specific protocols and guidelines. To start, a pre-survey was administered to assess the staff's baseline comfort and preparedness when floating and asked them to rate their level of clarity on specific processes that are unique to each unit. Analysis of the pre-survey revealed that staff, more often than not, felt somewhat or completely unprepared when floating. Additionally, about 25% of floats stated their clarity on specific unit practices was either somewhat or very unclear. Once the baseline data was analyzed, the Float UPC, with support from leadership, collaborated with Professional Governance Councils to engage each unit to participate and complete their dedicated tip sheet. Each unit received a Qualtrics link with a template containing sections staff determined useful when floating. The original aim was to use a QR code to access the tip sheets. However, this aim quickly changed during COVID as the staff needed their personal device to scan the code and locate the information. Due to the code's challenges, a collaborative effort with the ISS team helped shift the implementation strategy, and a unique float pool website was created to rehouse the tip sheets. Staff awareness of the project was promoted during staff meetings, weekly huddles, on-boarding, educational opportunities, and leadership rounding to encourage utilization. After nine months, a post-survey was administered to collect qualitative data, and the quantitative data were evaluated from the website's analytics to determine the use of the new website. The qualitative data showed that 83% of staff now reported being adequately prepared when floating vs. the 44% who reported somewhat or completed unprepared pre-tip sheet use. The quantitative data determined that 78% of web page viewers clicked on at least one tip sheet. Although we do not have pre-tip sheet webpage data since it is new, it can be implied that tip sheet usage could lead to improved patient care and outcomes due to increased staff preparedness when floating.
25-QI. Bundle It! Implementing Best Practice to Prevent Hypothermia in Neonates Born in L&D
Tabitha Benga
11/3/2022, 4:50pm - 5:20pm, Poster
In CY 2020, 7.1% of infants admitted to a Level IV Neonatal Intensive Care Unit from the Labor and Delivery Rooms (LDR) and Labor and Delivery Operating Rooms (LDOR) were hypothermic with axillary temperatures of <36.0°C. Neonatal hypothermia has shown positive correlation with higher rates of morbidity and mortality, as well as increased lengths-of-stay. A literature search of recent evidence and recommendations suggested that implementation of a hypothermia bundle and staff education leads to decreased rates of hypothermia. The aim of the project was to decrease the percentage of hypothermic infants admitted to NICU from LDR and LDOR to zero by the end of CY 2021 and sustain the hypothermia percentage below the national benchmark of less than 10% of infants. A monthly interdisciplinary taskforce reconvened to reevaluate current practices and determine the latest evidence-based practice improvements. After extensive review of the literature, the existing hypothermia bundle was updated to contain specific weight-based guidelines. For literature review, seventeen articles were reviewed consisting of all five levels of evidence (Level I systematic review/meta-analysis, Level II randomized control trials, Level III-controlled trials without randomization, Level IV case control/cohort study, and Level VI qualitative studies). Practice changes in the timing and frequency of obtaining axillary temperatures were implemented. Taskforce members performed root cause analyses (RCA) of past hypothermic cases in 2020. With the RCA data, an audit tool checklist was created that gathered information on each hypothermic admission and the barriers that may have been encountered. In summary, hypothermia was mainly attributed to the low ambient temperature in LDR and LDOR, the use of unheated air during resuscitation, and a staff knowledge gap. The taskforce collaborated with L&D staff members to address delivery rooms ambient temperature. After consulting with the Infection Prevention team and L&D Providers, baseline delivery room temperature was increased from 68 degrees to 72 degrees. Additionally, the team trialed and currently is in the process of purchasing new equipment that provides heated and humidified air in LDOR during resuscitation. Staff knowledge gaps related to hypothermia best practices were identified and addressed through extensive NICU and LD staff education by taskforce members using face-to-face teaching and distribution of visual resources. After implementation of all measures, submitted audit tools were reviewed monthly with RCAs done on any new hypothermic admission. Hypothermia rates decreased from 7.1% in CY 2020 to 4.8% in CY 2021 as a result.
45-R. Nurse Leaders Perceptions of Challenges and the Strategies in a Post-Covid-19 Environment
Nancy Ballard
11/3/2022, 4:50pm - 5:20pm, Poster
Nurses across the professional spectrum are working harder and in new ways due to systemic changes caused by the Covid-19 epidemic. Capturing the challenges, innovations, practice models and processes developed to deal with the changing healthcare environment is an important area for research. The current nursing shortage and projected future shortage have contributed to the negative impact on quality and operational outcomes. Collection of information on the current state can facilitate the ability of nurse leaders to be the change agents needed to regain the pre-Covid-19 momentum in improved outcomes important to high quality healthcare. Nurse leaders from all levels are uniquely positioned to provide insight into the current challenges, identify root causes, and obtain feedback from clinical nurses needed to develop strategies for change at system, organization, and unit levels. A better understanding and prioritization of challenges through the lens of the nurse leader is vital for planning best use of current resources and planning for the rebuilding of the nursing work force. Purpose: The purpose of this study is to describe the current challenges that nursing administrators face and the strategies they use to offset the challenges. The following research questions are driving this study: 1. What do nursing leaders view as their most pressing challenges? 2. What strategies do nursing leaders use to address these challenges? Methods: This is a descriptive cross-sectional study examining the challenges and strategies that nursing leaders face and use at the current time. Sample & Setting: Data will be collected via confidential online social media surveys including Facebook and Twitter, and email listservs. To be eligible for the study, potential participants must be: a) a nurse leader at a nurse manager position and above, such as a nurse manager, director, chief nursing officers, and chief executive officers, and b) 18 years of age older. The anticipated sample size is about 500 or more who will complete the survey. Instruments: Demographic form- age, ethnicity, education, current position, years as a nurse, and years as a nursing administrator The World Health Organization-Five Well-Being Index (WHO-5) to measure current mental well-being (time frame the previous two weeks). Two open-ended questions: 1.Please list the top 3 challenges you face currently, in order of priority with 1 being highest priority. 2.Please list the top 3 strategies you are currently using to address each of these challenges Results: Data will be analyzed using quantitative and qualitative descriptive methods. We anticipate completion of data collection by June 30, 2022 with analysis completed by September 30, 2022. Abstract will be updated with findings when analyses are complete.
80-ASP. Building Community & Sharing our Strengths: Collaborating as Nurse Educators in Academic and Practice
Molly Jackson
11/3/2022, 4:50pm - 5:20pm, Poster
Submission: Academic-Service Partnerships (ASP) Title: Building Community & Sharing our Strengths: Collaborating as Nurse Educators in Academia and Practice Problem: A need was identified for professional development for nursing professional development specialists (NPDS) at a 23 hospital health system. This initiative aims to strengthen academic-practice educational collaboration and leadership in nursing to promote competency in practice and promote scholarship in nursing education. Evidence Appraisal and synthesis: A literature search was conducted utilizing CINAHL, PubMed, and EBSCO from 2010 to 2022. Keywords included: Academic Nurse Educator, Nurse Professional Development Specialists, Academic Practice Partnerships, Nursing, Education Only one publication specifically addressed educational partnerships between academic educators and NPDS and was related to curricular development. Implementation Strategies: Through consultation with the System Director of Nursing Education of a 23 hospital health center and an academic faculty member of a midwestern nursing school, professional development for the NPDS was identified as a priority. A learning needs survey based on the Scope and Standards of NPDS (NPDS, 4th ed., 2022) had previously been conducted. A focus group with 25 systems-level NPDS provided further understanding of specific, timely educational needs in light of the current climate post-pandemic. Four general education themes were identified, with a half-day seminar planned by two academic faculty to address foundational educational theory and practice, including: 1. Knowing your Learner 2. Backward design 3. Engaging the Learner 4. Evaluation Methods All NPDS for the health system were invited, with a Continuing Education Certificate awarded upon completion. The session was held on April 22, 2022. Evaluation: Fifty-one nurse education leaders from the hospital system attended the in-person session. The evaluations were very positive and indicated that the program objectives were met. Each participant identified at least one change they planned to make in their planning, course design or evaluation process. In addition, many requests were made for future professional development topics. Lessons Learned: Attendance and feedback revealed a strong interest in offering development opportunities for NPDS. Opportunities to develop nurse scholarship was a theme identified by a number of the participants, which will add to the Science of Nursing. The next steps and implications will be described in greater detail at the ALSN Conference.
5-EBP. Nursing Leadership Mission Critical Checklist
Angela Prestia
11/3/2022, 4:50pm - 5:20pm, Poster
A novel solution to tackling the myriad of nursing leadership challenges was developed. Grounded in evidence, the Nurse Leader Mission Critical Checklist provides essential elements in a sequential order. The IHIs quadruple aim provides the framework for nurse leaders to focus their attentions on assuring, population health, patient satisfaction, as measured by safe quality outcomes, decreasing health care costs, and improving staff practice environments. Additionally, nurse scholars tout the importance of self-care, relationship building and sustainment, and the importance of preserving patient and staff human dignity. The Nurse Leader Mission Critical Checklist assists with memory recall, to reduce vulnerabilities. Developed to be used daily, it can assist nurse leaders in decreasing the possibilities of missed opportunities.
83-EBP. A Fierce Change for Nursing Leadership
Elizabeth McNulty
11/3/2022, 4:50pm - 5:20pm, Poster
Communication plays a key role in patient safety (Anbari et al. 2019). The IOM challenges nurses to develop a new workplace culture that encourages and supports leaders to hold each other accountable for the teams performance. AONL states the nurse leaders role is influential in creating a professional environment and fostering a culture where interdisciplinary team members can contribute to optimal patient outcomes and grow professionally (AONL, 2015, p.3). Fierce Conversations, a communication development program designed to improve communication and accountability has been offered at this institution since 2016. The goal of the program is to increase nurse satisfaction, engagement and improve the overall working environment. Less than one third of all nurse leaders have attended Fierce and there is no standard way of how leaders provide feedback. The inquiry for this EBP initiative is if nurse executives are educated in Fierce Conversations, will a top-down approach to change promote open communication, consistency and accountability. A structured literature review driven by the PICOT question; for nurse leaders how does Fierce Conversations education impact knowledge of communication strategies? was conducted utilizing four databases. The design is a quality improvement project and will be implemented in the summer of 2022. Kotters 8 steps of change will used as the theoretical underpinning for this initiative. Strengths of this model that make it ideal for the Fierce change in nursing leadership are the emphasis on the sense of urgency, the top-down approach, the volunteer army, and sustainability. By encouraging open communication, speaking up and fostering trust, nurse leaders can create a culture of patient safety (Labrague & De los Santos, 2020). Outcomes will be reported and available in the fall of 2022. The anticipated outcome is that Fierce Conversations will improve accountability and patient safety by educating and coaching nurse executives on providing feedback, promoting open communication and speaking up among nurses.
65-EBP. A National Evidence-based Implementation Project Leading Age-Friendly Care in Convenient Care
Mary Dolansky
11/4/2022, 10:45am - 11:45am, Breakout 11
In 2018, MinuteClinic, a national convenient care organization, started their journey to become an Age-Friendly Health System (AFHS) Committed to Care Excellence in an academic-practice partnership with the Frances Payne Bolton School of Nursing. The Institute for Healthcare Improvement (IHI) evidence-based AFHS 4Ms Framework and Guidebooks were used with the goal to reliably deliver the 4Ms as a set - What Matters, Medications, Mentation, and Mobility- to every adult 65 years of age and older receiving care at the MinuteClinic (except vaccine and urgent visits). What Matters is integrated into the clinic by asking the patient at the start of the visit What Matters and aligning the treatment plan at the end of the visit. Medications are integrated using an electronic health record enhanced medication reconciliation system that flags medications that are on the American Geriatric Society Beers Criteria. Mentation is assessed by using the PHQ2 and the Mini-Cog 3-minute assessment. Mobility is assessed as the patient enters the room and sits down as a Modified Get-up-and Go test. The visit is facilitated by using a patient-centered brochure at every visit to facilitate consumer communication about the AFHS movement, provide information on health promotion, and facilitate communication with primary care providers. The project is led by the MinuteClinic Quality Department and embraced as a quality initiative of implementing evidence-based care. A one-year planning period to develop a process-flow map, educational materials, practice-based tools, and electronic health record (EPIC) alignment was followed by an 11- month implementation phase starting June 1, 2020, in spite of the COVID-19 Pandemic. MinuteClinic became an AFHS Participant in June 2020, with the launch of the 4Ms Orientation to its ~3000 APRNs in 33 states and DC. The Committed to Care Excellence metric in the MinuteClinic was measured by regions meeting the delivery of the 4Ms as a set for three consecutive months. The MinuteClinic has achieved Committed to Care Excellence for all regions. Statistical process charts demonstrates the impact on the counts for each of the 4Ms uptake over time and the rate of improvement on delivering the 4Ms as a set. Implementation strategies used include professional development, marketing strategies Regional Age-Friendly Champions, electronic health record enhancements (best practice alerts and dashboards). Exploratory analyses using a t-test to examine significant differences in each of the 4Ms in baseline vs. intervention (two sample, unequal variances). Significant improvements were noted for all 4Ms (What Matters, Medications, Mentation, and Mobility, p<0.05 when comparing the intervention to baseline time periods. Continued efforts to implement booster strategies is underway to ensure that Age-Friendly care is delivered reliably to older adults by 3000 APRNs in 35 states and the District of Columbia.
24-R. Resiliency and Health in Nursing: An Intra-COVID-19 Replication Study
Mikel Hand
11/4/2022, 10:45am - 11:45am, Breakout 11
Problem/Background/Rationale: The nursing profession in the United States and globally is facing significant challenges in maintaining an adequate supply of nurses to meet the care demands of consumers. These challenges stem from several factors. At the present time, COVID-19 is the stimulus for many of these including those associated with resiliency, physical health, and mental health. Purpose/Aims/ Goals and Objectives: Purpose: The purpose of this study was to examine the post-Covid-19 state of resiliency, mental health, and physical health of nurses in a rural community, Magnet-Designated Organization, and to assess for changes in baseline levels of health and resiliency in the population from data obtained during a pre-Covid-19 assessment. Aims: The 1. To examine resiliency and perceived physical and mental health status of registered nurses working in a rural, Magnet-Designated Hospital pre and post Covid-19 using descriptive analysis. 2. To compare results from a pre-Covid 19 assessment of Resiliency and perceived physical and mental health with current findings. The following research question was posed in this study: 1. How has the Covid-19 pandemic impacted the degree of self-perceived resiliency, physical health, and mental health present in the registered nurse workforce in one rural, Magnet -Designated Hospital? Methods, Collaboration, Implementation, and Evaluation: This study was approved by the facility institutional review board. A descriptive design was used for the study. The setting was a rural Magnet-designated hospital in Southeastern Indiana. A convenience sample of (N=248) registered nurses employed by a rural Magnet-Designated hospital were invited to participate in the study. Each nurse received a Qualtrics survey that also included information concerning the study, risks, and benefits, and that participation was voluntary. Participants were asked to complete the survey at one time. 136 (55% response rate) completed the survey. The survey included a demographic questionnaire. Resilience was assessed using the Connor Davidson Resilience Scale. Self-perceived physical and mental health status was assessed using the Promis Global Health Short Form v. 1.1. Data were analyzed using STATA MP 14.0. Independent two-sample t-tests were performed to compare the differences between the pre-and post-survey respondents for continuous variables (i.e. age, resiliency score, physical and mental health scores), A p-value <.05 was considered statistically significant. Results, Outcomes, Implications: Analysis of Pre and Intra-Covid mean scores indicated a decline in resiliency scores (p=.0339). Analysis of perceived physical and mental health scores revealed a statistically significant decline in both Physical Health Scores (p < 0.0001) and Mental Health Scores (p = .03338). The results of this study reveal alarming trends for resiliency, physical health, and mental health in the RN workforce that comprised this study sample. All three study endpoints showed statistically significant declines in the analysis of pre and post-Covid-19 data. Even more alarming is that these findings align with the nationwide and global RN workforce trends discovered in the review of the literature. It is imperative that tailored interventions be developed to address these declines.
89-ASP. Developing Business Skills and Financial Acumen of Nurse Leaders
Nancy Manning Crider
11/3/2022, 4:50pm - 5:20pm, Poster
Many nurses are promoted to management positions without adequate financial background or education. This is particularly apparent in middle managers. The American Organization for Nursing Leadership (AONL) Nurse Executive Competencies (2015) and the AONL Nurse Manager Competencies (20150 delineate the knowledge, skills, and abilities of nurse leaders in executive practice. These competencies were developed in conjunction with the American College of Healthcare Executives and other organizations that comprise the Health Care Alliance. The competencies include not only communication and relationship management, leadership, and professionalism, but also knowledge of the healthcare environment and financial business skills and principles. It is clear that the nursing profession must enhance its business acumen to continue to advance as a credible leader of the rapidly evolving and complex healthcare delivery system of the future. The American Association of Colleges of Nurses (2021) The Essentials: Core Competencies for Professional Nursing outline the curriculum learning experiences that are needed for nurse leaders at all level of practice and how these experiences are integrated across the curriculum. The essentials define competency-based education as a process whereby students are held accountable to the mastery of competencies deemed critical for an area of study (ANCC, 2021, p4). A competency-based curriculum uses technology and other advanced experiential learning approaches that link learner outcomes to observable behaviors (AACN, 2021), The purpose of this presentation is to share information about key courses in the DNP curriculum offered by the Cizik School of Nursing at the University of Texas Health Science Center at Houston. The courses are designed to prepare the graduate level learner to function as a business and strategic leader in health care settings, and a contributing member of the team in business, finance, organizational change, and strategic planning for the organization.
79-R. Front-line leaders fatigue and cognitive performance: what do we know so far?
Amany Farag
11/4/2022, 9:30am - 10:30am, Breakout 8
Front-line leaders, nurse managers (NM), and assistant managers (AM) are the backbone of hospitals' daily operations. By virtue of their position, they assume accountability for patient, nurse, and unit outcomes. However, with the ongoing nursing shortage and the most recent pandemic, front-line leaders are pulled to the bedside. A situation that subjected them to extensive fatigue, a major threat to their overall well-being. The concern about the well-being of healthcare providers has been growing but received a big push with the introduction of the Institute for Healthcare Improvement's Quadruple aim. Yet, most of the available studies aimed at evaluating nurse fatigue, with limited studies directed toward front-line leaders' fatigue in general and during COVID in particular. Furthermore, there are limited studies in both nursing and non-nursing evaluating the relationship between front-line leaders' fatigue and their cognitive function [decision fatigue and cognitive failure (attention, action, memory)]. The purpose of this descriptive cross-sectional multisite study was to evaluate front-line leaders' occupational fatigue and its association with their cognitive function. Data for this study were collected from a convivence sample of front-line nurse leaders (NM and AM) working in all in-patient and critical care units in two Midwestern hospitals. Data collection lasted from July 2020 to April 2021. The study participants completed the paper-based study survey using four valid and reliable self-report fatigue and cognitive function measures. To increase the response rate, three reminder flyers were sent to the study participants over a three-week period. Participants were compensated for their participation. Descriptive statistics and regression analysis were performed to address the study's purpose. The Cronbach's alpha scores for the used measures ranged from 0.78-0.94. The final sample comprised of 31 NMs and 45 AMs. There was no statistical significance difference between NM and AM in their fatigue and cognitive function levels. The study participants reported higher acute (M= 59.4, SD=24.4, 0-100 scale) and mental fatigue (M=3.0, SD=1.30, 0-6 scale) than chronic (M=45.9, SD=27.8) and physical fatigue (M=1.5, SD=0.99). Despite the elevated fatigue levels, to our surprise, our participants reported very low decision fatigue (M= 0.8, SD=0.56, 0-3 scale). Only one domain of cognitive failure (attention) was elevated (M=2.7, SD=0.86, 1-5 scale). Among various fatigue types, chronic fatigue was the strongest predictor of cognitive function (β=.28, p<.004 and β=.32, p<.003) for cognitive failure and decision fatigue, respectively. Front-line leaders suffer from occupational fatigue at levels comparable to what we have seen in our prior work with registered nurses. In fact, they displayed higher levels of chronic fatigue. This result shows that occupational fatigue is not contingent on shift work. Therefore, fatigue mitigation and wellness measures should be directed toward both front-line leaders and their staff. The positive result of maintaining cognitive function despite high fatigue requires further investigation of personal and organizational attributes supporting front-line leaders' cognitive performance. This information will inform possible wellness interventions. Replicating the study with a larger sample and with longitudinal data will provide added information about change over time.
59-EBP. Prevention of CAUTIs in hospitalized adults: An EBP initiative
Nimian Bauder
11/4/2022, 9:30am - 10:30am, Breakout 8
Catheter associated urinary tract infections (CAUTI) are one of the most common hospital acquired infections (HAI) and no longer reimbursable as of 2008. At least half of all CAUTIs are considered avoidable. CAUTIs increase hospital length of stay by 2-4 days, becoming costly to organizations, and account for more than 30% of acute care hospital infections. In 2020, organizational CAUTI rates at this organization were trending above the national benchmark. This organizations practices included use of a CAUTI bundle. One gap identified by leaders included lack of a decision tree to guide practice, as registered nurses (RN) did not always know the indication or necessity of the urinary catheter. The infection preventionist and medical providers were relied upon to request urinary catheter removal when no longer indicated. Leaders of the team also identified the need for empowerment strategies based on best practices in the literature. Use of a CAUTI bundle was a primary recommendation described in the articles, which was already utilized at this organization. Additional recommendations included 1) use of a visual decision tree to guide catheter removal, 2) improved criteria for insertion and catheter necessity, and 3) empowerment strategies in which nurses advocate for catheter removal according to best practice. The purpose of this EBP initiative was for the RN to use a decision tree to identify proper indications for use of indwelling catheters and to empower them to advocate for patients by initiating conversations with the providers about catheter removal. The framework used to guide the implementation was the Helene Fuld 7 steps of EBP and ARCC Model. The team developed a decision tree using findings from the literature review. This decision tree helps nurses quickly identify appropriate indications for placement of indwelling catheter and reminds the nurse of the CAUTI prevention bundle. CAUTI nurse champions assisted in the implementation of the decision tree by introducing the new process during huddles. Posters describing the new process were hung on each nursing unit to reinforce the change. The concept of empowerment was reinforced throughout with support from leaders, providers, and team members. These efforts were strong facilitators of the EBP change. This EBP initiative drove NDNQI CAUTI rates below the national benchmark in 4 consecutive quarters to date.
81-R. Nurse Acceptance and Use of Continuous Vital Signs Monitoring (CVSM) for Adult Medical/Surgical Patients
Sarah Knowles
11/3/2022, 4:50pm - 5:20pm, Poster
The expansion of increasingly complex use of technology for direct clinical care offers both benefits and burdens for nurses in delivering safe and effective care. While continuous vital signs monitoring (CVSM) has been a standard of care in critical care, CVSM is a relatively new concept in both the patient home and acute inpatient setting. CVSM offers timely detection of clinical deterioration in patients in acute care in comparison to detection by standard intermittent vital signs measurements. However, the successful application of CVSM technology in assessing patients depends on nursing staff as end users. The Unified Theory of Acceptance and the Use of Technology (UTAUT) describes principles of staff use and engagement with technology including: performance expectancy, effort expectance, social influence, and facilitating conditions. Drawing on the UTAUT the purpose of this study is to assess the relationships among those factors that determine the intention to use Continuous vital signs monitoring in adult patients on general medical surgical units. These determinants of acceptance by nurses towards this technology will be applied to supporting the adoption and usage of this technology with adult patients in the medical/surgical care areas. The research questions include: Q1: What are the relationships among performance expectancy, effort expectancy, social influence and facilitating conditions with intention with intention to use? Q2: To what extent does performance expectancy, effort expectancy, social influence and facilitating conditions predict intention to use? Q3: Do personal and professional demographics influence performance expectancy, effort expectancy, social influence, facilitating conditions and intention to use? This descriptive correlational study is based on an online survey of nursing staff of an academic medical center who work on medical surgical units where CVSM technology is scheduled to be implemented. All registered nurses (n = 197) and nursing assistants (n =143) working full time or part time will be sent a link to the REDCap survey. Personal and professional demographic characteristics are collected. Performance expectancy, effort expectancy, facilitating conditions are measured using Venkatash et al, 2003 16 item measure of the UTAUT. A sample size of 128 (37% response rate) is needed to adequately power the study. With IRB approval, recruitment outreach will include announcements at staff meetings, emails with timed follow-up reminders and printed flyers posted in units. Data will be analyzed using univariate and multivariate statistics. Survey items will be grouped by UTAUT principles, and results will be compared across demographic characteristics such as professional role or full/part time status, using T-test, ANOVA, or Chi-square analyses. The analysis will show the acceptance and intended usage of CVSM among nurses and nursing assistants working on medical surgical units in five acute care hospitals within UH system. The results of the study will contribute to the science of nursing through publication on the application of the UTAUT theory to direct patient care technology. Implications for nursing will include support for nursing leaders looking to implement technology, targeted areas of focus with adoption of new technology and base for spirit of inquiry for new research.
31-R. Evaluating the Feasibility of a Mini-Mindfulness Intervention for Nurse Leaders during the Pandemic
Rebecca Owens
11/5/2022, 9:30am - 10:30am, Breakout 20
Problem/Purpose: For nurses, practicing and maintaining a state of mindfulness, even briefly, has been shown to help reduce compassion fatigue, burnout, secondary traumatic stress, anxiety, depression, while reducing errors, improving patient outcomes, resilience, and empathy. Mindfulness based interventions (MBIs) appear to be a promising target for cultivating resilience and reducing burnout, but solutions pertaining to their dissemination and actionability remain uncertain. Most nurse MBI research involves outcomes from 8-week sessions of 2.5 hours each week combined with daily individual practices. Because of the extent of time required there is a high dropout rate. Considering these burdensome intervention requirements, more data is needed on the minimum dose of mindfulness for achieving positive outcomes such as an MBI that can be readily implemented during work hours. Few studies have examined the effectiveness of shorter interventions. Specific Aims: Evaluate the feasibility of implementing a 3-minute MBI with nurse leaders practicing during the pandemic and assess self-reported stress before and after use of the intervention. Design and Methods: The intervention included a customized YouTube link of a three-minute mindfulness-based breathing space, the 3MBS, that was created and distributed by the researchers to all participants. The 3MBS intervention begins with a three-minute breathing exercise: one starts with simply the watching of thoughts, from moment to moment, as though watching them on a large movie screen. Then letting go of this wide view, the second minute is more narrowly focused on breathing in the region of the body that is most noticeable for the individual (nostrils, throat, chest, etc.). Lastly, in the final minute, ones attention moves to the body as a whole, allowing the individual to become aware of body sensations present in the body and the current moment. The 3MBS process flow mirrors the shape of an hourglass. Nurse leader volunteers were recruited from east and west coast environments to test the feasibility and effectiveness of the use of the 3MBS among nurse leaders practicing during the pandemic. Results: While many of the nurse leaders reported use of the 3MBS twice/day, there was inconsistency in use among participants. Those who used the intervention reported a decrease in the stress levels post intervention. Conclusion: Given the benefits shown in this preliminary study of 3MBS, there is room for embedding and expanding this new and empirically validated intervention into nurse leaders work life. Additional research with specific targeted outcomes is warranted.
22-R. An Exploration of Frontline Nurses Managers Experience during the 2020 COVID-19 Pandemic
ESTHER CHIPPS
11/5/2022, 12:00pm - 1:00pm, Breakout 26
Nurse leaders are facing great challenges during the COVID-19 pandemic. Insufficient empirical evidence exists to fully understand the extent of the pandemic impact on nurse managers. The findings from this qualitative study indicate that there are rapidly escalating stresses among NMs that are seriously impacting job satisfaction and retention.
70-R. A new framework for rebuilding healthy practice environments: What team virtuousness looks like in healthcare teams
Lynn Varagona
11/5/2022, 10:45am - 11:45am, Breakout 23
Background: Nurse leaders (i.e., nurse managers and above) experienced burnout, incivility, hopelessness, ethical challenges, and high turnover among themselves and their staff during the COVID-19 pandemic. Amid these challenging times, nurse leaders asked for evidence-based practices to improve the practice environment. When practice environments are healthy: a) nurses experience less burnout, b) job dissatisfaction and intention to leave among nurses are lower, and c) quality of nursing care provided is higher. Healthy practice environments can be fostered by virtuous leadership, however minimal guidance exists regarding what virtuous leadership looks like. Virtue ethics may provide such guidance. Purpose: The purpose of this review was to evaluate and summarize the nursing virtue ethics literature and examine how virtue ethics has been applied to healthcare teams. The overall research question was: How is virtue ethics incorporated into nurses healthcare team research? Methods: An integrative review of scientific literature on the topic of virtue ethics and nursing was conducted in March 2022. PRISMA guidelines were used to search CINAHL, Pub Med, Google Scholar, ProQuest, Ovid, Medline, Health & Medicine Gale, and Health Source: Nursing / Academic Edition. Key terms used for the database searches were virtue ethics AND nurs*. No date limit was set for the review. After the initial review yielded only a few studies, an emerging synthesis approach was used. Since most of the articles were not research, concept analyses, reviews, opinion and position papers, and grey literature were included according to the inclusion and exclusion criteria. The level of evidence and quality of articles were assessed using the Johns Hopkins tools. Results: Twelve articles were found relevant to the topic of virtue ethics and nursing. Hand searching led to two additional articles. Research studies were limited to two. Most of the non-research articles pertained to debating whether virtue ethics belongs in nursing. Regarding research articles, Smith and Godfrey conducted a qualitative study of 53 nurses from a convenience sample of volunteers at a nursing ethics conference. They concluded elements of virtue ethics aligned with characteristics of a good nurse and good nursing was an extremely complex concept that warranted further investigation. Varagona and Ballard used exploratory and confirmatory factor analysis to uncover a reliable framework for team virtuousness on hospital units based on Aquinas Virtue Ethics Theory. Team virtuousness varied significantly among hospital units and had a moderate, positive, significant correlation with unit staff engagement. Conclusion: Virtue ethics has been of interest to the nursing community predominantly as a concept. There is a dearth of research on virtue ethics and nursing. One study uncovered and validated a new framework for virtue ethics in healthcare teams. Implications for Nursing Management: Varagona and Ballards new team virtuousness framework can guide nurse leaders in modeling virtuous characteristics and behaviors and coaching their teams to do the same. Doing so holds the promise of rebuilding strong, healthy work teams during these challenging times and realizing benefits of team virtuousness reported in the social sciences literature.
58-R. Role of Magnet-recognized hospital nurse managers in implementing evidence-based practice: A mixed-method study
Della Mathew
11/5/2022, 10:45am - 11:45am, Breakout 23
Role of Magnet-recognized hospital nurse managers in implementing evidence-based practice: A mixed-method study Della Mathew, Ph.D., PGDHA, EDHI, RN; Sandra K. Cesario, Ph.D., RNC-OB, FAAN; Ann Malecha, Ph.D., RN, CNE, PHNA-BC, CPH; Robin Toms, Ph.D., MN, RN, NEA-BC. Healthcare systems recognize evidence-based practice (EBP) as the prestigious standard for providing safe and high-quality care. Implementation of EBP is essential for Magnet-recognition and is a hallmark of nursing excellence. Despite the well-documented benefits, implementation of EBP at the point of care is inconsistent and remains elusive in the United States and throughout the world. Although research is available to inform nursing practice, many patients still fail to receive evidence-based care. Implementation of EBP is a complex and challenging process. The literature review revealed a huge gap between nursing science and practice but provided evidence that nurse managers (NMs) had a pivotal leadership role in implementing EBP at the bedside. The purpose of the study was to gain a deeper understanding of the leadership roles, their influencing factors, and the experiences of Magnet-recognized hospital nurse managers (MRHNMs) in implementing EBP in their units. This mixed-method study was based on Goodalls (2016) Theory of Expert Leadership to examine the roles of MRHNMs in implementing EBP. A sequential explanatory method with a quantitative-driven design based on a national correlational survey augmented a qualitative descriptive component using semi-structured interviews. The study targeted critical care and acute care NMs of all Magnet-recognized hospitals in the United States. The data was collected with the Implementation Leadership Scale (ILS) and the interview guide. Correlations, multiple regression, and Creswells content analysis answered the research questions. The results reported a moderate level of leadership roles (54.6%) of MRHNMs in implementing EBP, and produced numerous themes indicated that, in fact, NMs did implement EBP with struggle. The prominent themes discovered in the qualitative data analysis upheld and enhanced the findings from the survey. MRHNMs viewed EBP as a healthcare priority and the leadership of NMs is necessary to promote the implementation of EBP. However, lack of knowledge, difficulties with the EBP process, time constraints, and staffing issues negatively impacted EBP. Factors that enhanced the implementation of EBP included post-graduate NMs, formal EBP education, working in critical care units, collaboration with doctorally prepared nurses, and Magnet organizational culture. The leadership of MRHNMs is necessary to shape evidence-based care at the bedside and at an organizational level to sustain Magnet-recognition.
77-QI. Implementing a multimodality, multidisciplinary approach to novice nurse success in the Emergency Department
Rocio Garcia
11/3/2022, 2:30pm - 3:30pm, Breakout 5
University Hospital (UH) in San Antonio, Texas is a Magnet designated facility and the primary academic partner for University of Texas Health San Antonio. As the regions only combined pediatric and adult level 1 trauma and academic medical center, the emergency departments (ED) average over 87,000 visits annually. Historically the ED at UH utilized a standardized approach to novice nurse (NN) orientation. Orientation included 12 weeks with a preceptor, bi-weekly meetings with the educator and completion of competencies. In late 2019, an analysis revealed deficiencies in the orientation process resulting in significant NN turnover and overall dissatisfaction. High NN turnover results in negative outcomes such as decreased staff morale, decreased quality patient care, and preceptor burn out. These outcomes have effects on operations and quality throughout the health system such as financial losses that can exceed $120K per NN and an increase in patient safety events. A review of evidence through CINAHL, PubMed and the Cochrane library recovered 25 articles using keywords new nurse orientation mentor, and education. Filtering for dates from 2010-2020 returned 10 articles used for development of a new orientation. They consisted of a systematic review, a quasi-experimental study and a randomized experimental study. The remaining evidence were program reviews and expert opinions. The quality improvement (QI) project stemmed from the PICOT question: Will updating the current novice nurse orientation to a multimodality and multidisciplinary approach improve retention and confidence in their clinical practice within one year? The QI project goals were decreased patient safety events, increase nurse retention, and improved confidence in their nursing practice. In 2020, the Multimodality and Multidisciplinary Approach for Novice Nurse Success (MMANNS) was implemented. The MMANNS orientation is a program that includes 20 weeks with an experienced preceptor on the unit and bi-weekly check-ins between nursing educator, orientee and preceptor utilizing the independence rating scale. Additional requirements include attendance at emergency medicine resident grand rounds and monthly multidisciplinary lectures, completion of medication reviews, and 40 + hours of the Emergency Nurses Association: Emergency Nursing Orientation online modules. Rapid Plan-Do-Study-Act (PDSA) cycles were completed in order to implement each modality. The planning phase of the PDSA cycles included process mapping and completion of a fishbone diagram. Participants included recent NN, resident physicians, pharmacists, respiratory therapists and nursing leadership (educators and directors). The multidisciplinary approach resulted in developing a collaborative orientation for the NN. Novice Nurse turn-over rate decreased from 53% to 16% within six months of independent practice post implementation of MMANNS. Use of the independence rating scale throughout the NN orientation demonstrated measurable growth in knowledge, skill and self-confidence. Concurrently patient safety events have also shown a steady decrease. Evaluation of results demonstrated effectiveness of new process to meet all goals and continued improvement. Implications: MMANNS provides variety of learning environments for addressing learners needs while improving peer communication and relationships.
93-R. The Conceptual Model for Professional Identity in Nursing: Academic-Service Implications
M. Lindell Joseph
11/5/2022, 9:30am - 10:30am, Breakout 20
The Conceptual Model for Professional Identity in Nursing is an active and transformative new mode of thinking for practice, academia, research, regulatory, and policy. How the professional nurse identity forms, remain to a large degree elusive to the profession. Using an action research design, the Conceptual Model for Professional Identity in Nursing was developed. The model promotes our understanding of professional identity by connecting nurses across all levels of educational preparation, roles, settings, and countries. The interconnectivity shown in the model, encourages collaboration, accountability, and sustainability for practice, academia, research, regulatory, and policy.
44-R. The Relationship between Collective Nursing Knowledge and Nurse Turnover: An Application of Nursing Intellectual Capital Theory
Pamela Russman-Chambers
11/3/2022, 1:15pm - 2:15pm, Breakout 2
The value of a healthcare organization is vested in the expertise, intellect, and wisdom of employees. Nursing knowledge resides both within the individual nurse and the collective knowledge embedded in organizational structures and practice environments. Healthcare organizations rely on their ability to utilize this knowledge to deliver high-quality care to patients. Hospitals wanting to gain a competitive advantage and achieve financial stability must be adept at acquiring, cultivating, and using the nursing knowledge stocks of the organization. When this knowledge can be utilized to mitigate healthcare issues and improve patients' health, this collective knowledge or intellectual capital is often the most critical organizational asset. Nursing intellectual capital is so vital because the work of professional nurses involves making critical life and death decisions. Like other intangible organizational assets, nursing knowledge is crucial to measure and manage to assist healthcare organizations in becoming high-performing entities. The purpose of this paper is to use a revised Nursing Intellectual Capital (NIC) Theory to evaluate the relationship between nursing intellectual capital and organizational performance, defined explicitly as nurse turnover. The revised NIC will be utilized to evaluate the relationship between quantitative measures of nursing intellectual capital and nurse turnover.
74-R. Relationships among Mentoring, Empowerment, and Organizational Commitment in Nurse Leaders
Meghan Weese
11/3/2022, 1:15pm - 2:15pm, Breakout 2
Engaged and empowered nurse leaders are needed to meet current and future healthcare needs. As nurse leaders are retiring or choosing to leave the profession, a better understanding of organizational commitment and retention strategies is needed. A supportive work environment for nurse leaders that provides opportunities for development is essential to grow and retain competent nurse leaders. However, investing in development poses a challenge to employer return on investment in terms of cost, time, and expertise if leaders who gain knowledge and skill leave to seek better employment opportunities. The reasons why nurse leaders stay or leave an organization is an area with little research. The literature suggests mentoring is a strategy for creating an empowering work environment leading to commitment; however, there is limited empirical evidence. The study purpose was to examine relationships among mentoring, empowerment, and organizational commitment in nurse leaders. The study was conducted using an exploratory descriptive cross-sectional correlational design with survey methodology. The study employed a convenience sample of nurse leaders (n = 167) recruited from membership of a statewide nursing leadership professional organization in the Midwest. Participants completed a survey containing demographic items and five valid and reliable instruments: Conditions for Work Effectiveness Questionnaire-II, Psychological Empowerment Questionnaire, Mentoring Practice Inventory, Mentoring Benefits Inventory, and Three-Component Model Employee Commitment Survey. Survey methodology aligned with Dillmans Tailored Design Method was used to distribute an online survey to the professional organization email list. Findings revealed the interplay of 20 moderate or strong positive and significant relationships among study variables in support of the proposed study model and contributed new knowledge that mentoring is positively and significantly related to empowerment and organizational commitment of nurse leaders. Mentoring practices and benefits had substantial or moderate positive relationships to structural empowerment and psychological empowerment in all areas. Workplace mentoring practices had a substantial positive relationship with structural empowerment and mentoring benefits, and a high moderate positive relationship with psychological empowerment, affective organizational commitment, and normative organizational commitment. Mentoring benefits were strongly correlated with individual mentoring practices, workplace mentoring practices, structural empowerment, and psychological empowerment, and moderately correlated with affective organizational commitment and normative organizational commitment.
67-R. Diverse experiences of organizational learning: A grounded theory study
Bret Lyman
11/3/2022, 2:30pm - 3:30pm, Breakout 5
Background Through organizational learning, nurse leaders can help their teams and organizations provide consistently excellent patient care and experiences, even in complex, dynamic healthcare environments. Through organizational learning, teams learn from their experiences, adopt evidence-based practices to improve quality of care, and successfully adapt to changes. As the nursing workforce becomes increasingly diverse, leaders must be more intentional than ever to ensure team members are engaged in organizational learning and are empowered to enact meaningful change. With effective leadership, ample education for team members, and a supportive organizational structure, diversity can improve a teams problem-solving processes, creativity, communication, and capacity for innovation, all of which are crucial to effective organizational learning. While many healthcare leaders and others may wish to foster organizational learning in diverse teams, there is a paucity of evidence to guide their efforts. Purpose The primary purpose of this study is to explore how individual differences and organizational context shape individuals experiences of organizational learning. A secondary purpose is to inform a subsequent longitudinal, qualitative study of individual experiences of organizational learning over time. Methods This is a qualitative, grounded theory study of how a diverse sample of Registered Nurses have experienced organizational learning. Up to 40 direct care Registered Nurses licensed in Utah or New Mexico are being recruited. Data are being collected through a brief demographic survey and semi-structured telephone interviews. Interviews will be transcribed verbatim. Member checking with selected participants will be used to add rigor to the analysis and clarity to the findings. A grounded theory approach will be used to analyze the data. Data collection and analysis will occur simultaneously. The open coding process will involve researchers independently reviewing the raw data, as well as identifying and labeling important concepts and events. To improve our theoretical sensitivity, we will collaboratively identify similarities and differences among our interpretations, allowing us to identify new concepts, refine labels for existing concepts and re-think how related concepts fit into various categories. We will then use an axial coding process to examine the categories in greater depth, describe each category in more detail, and refine the labels used for each category. We will then explore relationships among the categories and assign words or phrases that convey the essence of the related categories. We will continually refer back to the interview transcripts to ensure the themes accurately reflect the data. Selective coding will then be used to articulate the central phenomenon of the study. Ethical approval was obtained prior to recruitment and data collection. Results & Implications Results are pending, as data collection and analysis are currently underway. However, we believe the outcomes of this study will have important implications for nurse leaders. While many healthcare leaders and others may wish to foster organizational learning in diverse teams, there is a paucity of evidence to guide their efforts. A deeper understanding of how individuals experience and engage in organizational learning will equip leaders to create the diverse, inclusive teams necessary to provide excellent care for all patients.
42-EBP. Storytelling as a Pedagogy for Teaching Leadership Competencies
Todd Tussing
11/4/2022, 1:30pm - 2:30pm, Breakout 15
Storytelling has been a mode of teaching and learning for thousands of years. Human brains are wired to relate experiences and share meanings in the form of stories, and the art of storytelling has demonstrated its effectiveness as a pedagogy for learning. Healthcare leaders are challenged with sharing their learned experiences to novice leaders and students of leadership to help them grow as leaders and prepare for the challenges ahead. Intentional selection of the type of story leaders tell involves matching story to learning objective and must factor in ethical considerations when choosing the appropriate story.
76-R. Facilitating Organizational Resilience During the COVID-19 Pandemic: An Opportunity for Nurse Leaders to Effect a Crisis Leadership Response
Sonia Udod
11/4/2022, 1:30pm - 2:30pm, Breakout 15
The global onset of COVID-19 created an unprecedented and intense working environment for healthcare leaders around the world. The pandemic has placed unprecedented demands on healthcare systems by challenging regional and organizational capacity for infection control, rationing of healthcare supplies, and information management. Public health emergencies such as the COVID-19 pandemic have brought greater attention to crisis leadership (1), and placed intense psychological stress and pressure on the healthcare leaders, managers, and staff to make difficult decisions in a demanding work environment. The purpose of this study is to understand from senior healthcare leaders and front-line managers how crisis leadership was achieved, and organizational resilience was activated in the healthcare setting during the COVID-19 crisis response, and to learn from this for ongoing and future responses to health care crises. The qualitative exploratory research design consisted of criterion sampling of 14 senior health leaders and 10 frontline managers, across three health regions in Manitoba, Canada. Participants completed socio-demographic questionnaires and individual semi-structured interviews. Braun and Clarkes (2,3) six-phased approach to thematic analysis guided data analysis. Findings revealed various factors influencing crisis leadership and organizational resilience. Findings from senior healthcare leaders revealed the overwhelming nature of the global pandemic. The situation significantly impacted their operation, practices, and priorities. Some of the leadership challenges included the management of information, inadequate logistical processes, changing practices and protocols, and significant emotional distress. However, leadership engagement strategies also emerged. Health leaders also adapted by addressing priority issues, reforming structures and processes, and re-directing resources. For front-line managers, significant themes that arose from their responses also included experiences of significant emotional distress, changing priorities and practices/models of care, self-care management, and focusing on team cohesion and collaboration. Overall, numerous lessons were learned for enhancing organizational resilience and capacity building such as adopting an agile and compassionate leadership model, effective communication, innovation in changing care practices, and creating a readiness plan for future crisis and post-crisis behavior. Findings demonstrated how health leaders and managers can more effectively lead during a crisis for the short- and long-term. These findings have implications for retaining existing leaders and managers in positions of leadership and serve as a catalyst for organizational resilience.
52-ASP. Preparing an Implementation Science-Ready Nurse Leader Workforce
Heather Nelson-Brantley
11/4/2022, 2:45pm - 3:45pm, Breakout 18
Nurse executives are increasingly embracing evidence-based practice (EBP), yet it still takes 17 years to move just 14% of research into practice. The context for moving research into practice in healthcare systems is extremely complex. What works on one unit often does not translate to others, or may take hold initially but fail to demonstrate sustainable practice change. Implementation science is a multi-disciplinary, multi-sector, research-practice field that aims to understand how to move evidence-based interventions, innovations, and policy into everyday practice. Thus, it holds promise as a new solution for addressing ongoing challenges for nurse leaders. Nationally, calls have been raised for stronger academic-practice partnerships(2) and PhD-DNP collaborations. Yet, PhD nursing students continue to be trained in traditional research methods such as qualitative, quantitative, cross sectional, and experimental designs, devoid of collaborative research-practice learning opportunities with DNP students. Nursing PhD programs lack courses on new methods in implementation science that were developed for understanding how to move evidence into practice. Additionally, DNP-prepared nurse leaders are charged with moving evidence into practice, yet DNP programs lack courses in implementation science. Implementation science has the potential to help nursing realize its vision for strong academic-practice partnerships, led by PhD-DNP implementation science teams. To realize this potential, nurse leaders in practice must gain essential competencies for supporting implementation research and practice in their organizations, and nurse leaders in academe must concurrently focus on integrating implementation science into PhD and DNP curricula. This session will: 1) differentiate EBP, translational science, and implementation science; 2) identify essential leadership competencies for supporting implementation research and practice; and 3) share one nursing schools solution for integrating implementation science into PhD and DNP curricula through an innovative, inter- and intra-disciplinary PhD-DNP course in implementation science. Presenters will share how the course was designed, its content, learner projects, and evaluation of the course to date. Additionally, presenters will share resources with session attendees that they can use to build their organizations capacity for implementation science.
85-R. Navigating the Impostor Phenomenon: The Lived Experience of Nurse Leaders
Arzu Adiguzel
11/3/2022, 2:30pm - 3:30pm, Breakout 6
The Institute of Medicine identifies nurses as being in a position to become a powerful force for change in our healthcare system through their leadership. The impostor phenomenon is a psychological pattern in which individuals doubt their skills, talents, or accomplishments, or may have internalized fears of being exposed. In a time when nurse leaders are needed the most, these feelings may prevent nurses from advancing their careers and to lead. While a plethora of studies have examined this phenomenon and its negative impacts to mental health and career progression, there is little on the experience among nurses and none among nursing leaders or how to manage it effectively. Fellows of the American Academy of Nurses are considered nursings most accomplished leaders in education, management, practice, and research. These successful leaders have been recognized for their extraordinary contributions to nursing and health care. This qualitative study used a phenomenological method designed to gain insight into how these successful leaders have experienced impostor feelings. Ten nurse leaders were interviewed about their career progression, and their experiences with the impostor phenomenon were revealed. Findings were analyzed and the six essential themes that were illuminated from those shared experiences were: (a) Welcoming Opportunities, (b) Extended Sphere of Support, (c) Willingness to be Courageous, (d) Embracing the Journey, (e) Willingly Expressing Humility and Authenticity, and (f) Navigating the Impostor Process The findings from this study will contribute to the body of knowledge about the impostor phenomenon within the context of the nursing profession and leadership and may benefit other nursing professionals experiencing similar feelings to mitigate them in support of self-care. Importantly, the findings of this study strongly support advocating for, creating and sustaining healthy work environments. Recommendations for future research are also discussed. The most important implication of this study is that the nurse leaders perceived they were able to navigate impostor feelings successfully by establishing normalcy of those feelings, for example, through adopting the mindset that the feelings are transient and using humor and reflection. The essential themes (welcoming opportunities, extended sphere of support, and navigating the impostor process) emerged from the participants stories that they shared from their journeys in life. The research findings may imply that through a network of encouraging supporters, nurses can mitigate their IP feelings.
3-R. How COVID-Related Stressors and Work Environment Impact Burnout, Turnover Intention, and Resilience among Nurse Leaders during the Pandemic
Aoyjai Montgomery
11/3/2022, 1:15pm - 2:15pm, Breakout 3
Background and Significance: Even before the COVID-19 outbreak, at least one out of every ten nurses worldwide was suffering from high burnout, contributing to high turnover rates. Attributed to the COVID-19 pandemic, anecdotal reports of overwork, burnout, and even suicide of healthcare professionals is being shared in the news and on social media. The pandemic introduced new stressors to nurse leaders, e.g., managing the complex staffing situation (staff shortages, reassigning nurses to cover COVID-19 units, limited bed capacity, high patient acuities, shortage of personal protective equipment), while supporting their staff nurses. Since COVID-19 began, there has been research concerning COVID-related stressors, burnout, turnover intention, and resilience among nursing staff but not among nurse leaders. Research Objective: This study aimed to examine the COVID-related stressors and work environment that are most significantly related to burnout and turnover intention as well as how resilience impacts burnout and turnover intention. Methods: This descriptive, cross-sectional study employed an electronic survey of several instruments to measure COVID-related stressors (COVID-related Stress Scale: CSS), work environment (Nurse Manager Practice Environment Scale: NMPES), burnout (Copenhagen Burnout Inventory: CBI), turnover intention (a single item), and resilience (Connor-Davidson Resilience Scale: CD-RISC-25) among nurse leaders. In September 2021, 57 nurse leaders who worked in Birmingham, Alabama hospitals, including nurse managers, directors of nursing, and other nurses who are in administrative roles, responded to the survey. Principal Findings: The average respondent had 10.7 years of nurse leader experience, had a graduate degree (67%), and worked as a nurse manager (42%) or a nursing director (37%). All COVID-stressor subscales were negatively related to Culture of Generativity subscale of the work environment (defines as Nurse managers have adequate time to coach and develop their front-line staff) (r =-.24-(-.43), p < .05). The overall COVID-related stressor was positively related to all three burnout subscales (Personal, Work-, and Client-related Burnout) (r = .27-.40, p < .05) but not significantly related to resiliency and intent to leave (r = 0.17, p =.20). The overall work environment was negatively related to burnout (r = -.32-(-.68)) and intent to leave (r =-.28-(-.35)), but positively related to resiliency (r =.34-.59). Resiliency was negatively related to all subscales of burnout (r = -.53-(-.59), p < .01) and intent to leave (r = -.32, p < .05). Personal and Work-related Burnout were positively related to intent to leave (r = .30-.34, p < .05) Implications for Policy or Practice: Nurse leaders had to focus more on staff shortage issues and high patient acuities, and this could prevent nurse leaders from taking time to coach and develop their front-line staff. COVID stress impacts burnout but does not affect resiliency and intent to leave. The findings of this study provide baseline data to inform the development of actionable interventions to prevent or at least reduce burnout and turnover intention.
16-R. From Dissertaion to Program of Research
Nora Warshawsky
11/5/2022, 9:30am - 10:30am, Breakout 21
The purpose of this presentation is to provide guidance to novice nurse scientists seeking careers in academia. Research is critical to faculty success. Foundational decisions related to research can determine the degree of success years later. In this presentation, Dr. Warshawsky will share insights, strategies and recommendations for establishing and growing your dissertation topic to a program of research. This session is intended for PhD students and faculty in or seeking tenure-track positions.
86-R. ALSN Relational Leadership Research Collaborative: Relationships among Nursing Leadership Models of Authentic Nurse Leadership and Human-Centered Leadership, and the Transformational Leadership Model
K. David Bailey
11/5/2022, 9:30am - 10:30am, Breakout 21
As healthcare faces unparalleled changes in workforce dynamics and increasing complexity, nurse leaders must consider creating their own shift in how leadership is operationalized. While Transformational Leadership (TL), a relational leadership model borrowed from the business world, has been the healthcare industrys hallmark leadership style, perhaps the pandemic has illustrated that other relationship-based leadership styles may be more effective for nursing leadership and creating environments where nurses want to stay. Authentic Nursing Leadership (ANL) and Human-Centered Leadership in Healthcare (HCL-HC) are contemporary, evidence-based relational theories grounded in the essence of nursing practice. This research study provides a foundational psychometric comparison and analysis of TL, ANL, and HCL-HC and serves as the first of two phases of inquiry to explore the fit of relational nursing leadership approaches versus TL within nursing practice and their influence on intent to stay.
66-ASP. Creating and Evaluating Department-level Budgets
Nancy Crider
11/5/2022, 10:45am - 11:45am, Breakout 24
In 2010, the Institute of Medicines The Future of Nursing: Advancing Health, Leading Change report posited that nurses needed to prepare for leadership positions to more effectively lead change and advance health (IOM, 2011). In 2015, the Robert Wood Johnson Foundations Report in Brief: The Future of Nursing repeated this important message by suggesting nurses seek out additional preparation and education so that they were prepared to lead change and advance health (IOM, 2015). To support these initiatives, organizations such as the American Organization of Nurse Leaders (AONL), Sigma Theta Tau International, and the American Nurses Association (ANA) identified specific competencies that nurses and nurse leaders possess for them to adequately respond to the ever-changing challenges of todays healthcare delivery system (Morse & Warshawsky, 2021; Nghe et al., 2020). Interestingly, while many would conclude that opportunities are in place to allow nurses and nurse leaders to develop leadership competencies, Khoury et al. (2011) concluded that many nurse leaders do not possess the skills necessary to be viewed as business savvy leaders of the healthcare system. In fact, Warshawsky and Cramer (2019) posited that of the AONL nurse competencies, the competencies with the lowest scores included fiscal acumen and performance improvement, two entities that are critical for leading transformation in a healthcare organization. As a result, Raftery et al. (2021) concluded that the nursing profession needed to enhance its business acumen to evolve as a leader of the healthcare delivery system. Welch and Smith (2020) supported this conclusion as financial competency can provide a measure of independence and critical thinking imperative for the successful nurse leader. Through the application of financial skills, nurse leaders can manage productivity more efficiently and assess and proactively manage variances from a given standard (Welch & Smith, 2020). Thus, the purpose of this session is to educate interested participants in financial management with a specific focus on budgeting. Using problem-based learning as a basis, the session will focus on general budgeting principles and specific types of budgets followed by an interactive activity where the participants will be able to work in groups on creating and reporting a budget. Following the activity, the participants will be asked to report out suggestions and best practices to the group-at-large.
9-R. The Impact of COVID-19 on Nurse Managers Leadership Characteristics
Karen Fowler
11/3/2022, 2:30pm - 3:30pm, Breakout 6
Abstract Background- Nurse Managers are vital in improving nursing efficiencies and the quality of care provided during a crisis. They play a crucial part in creating a supportive environment promoting quality and organizational success. The value of positive leadership characteristics in managers has never been more critical than during the COVID pandemic. They are functioning in crisis mode required that nurse managers have clear communication and solid leadership skills. Therefore, nursing management, especially in emergencies such as the COVID-19, needs to be transformative in the sense that the manager is informational, motivating, and able to advance the organization, notwithstanding a global pandemic. Objective- The study aimed to investigate the leadership characteristics used by nurse managers during the COVID pandemic. Rapid implementation of changes required with the influx of patients and complexity of care during the COVID pandemic required resourceful nursing management. The nurse managers' competencies and leadership style impacted patient care provided during this time. Methods- An exploratory, quantitative study was conducted. The Multifactor Leadership Questionnaire (MLQ 5X) was randomly sent to registered nurses (RNs) in Texas using the state board listing of active RNs. Seventy practicing RNs participated in the study. Data analysis was conducted using descriptive statistics and multivariate correlational analysis. Results- Perceived leadership characteristics remained primarily transformational. However, compared to a U.S. normative sample, nurse managers demonstrated a significant decline in positive leadership characteristics. Linking Evidence to Action- Specific tactics and strategies must be adopted to support nurses and nursing managers during the ongoing healthcare crisis. Close monitoring of managers' leadership characteristics will enable organizations to support and provide educational opportunities for continued organizational success.
27-R. Moral Injury, Resilience, and Well-Being among Nurse Leaders during the COVID-19 Pandemic
Joyce Fitzpatrick
11/5/2022, 12:00pm - 1:00pm, Breakout 27
Problem: COVID-19 has brought increased occupational risk for nurses and other healthcare employees, including significant mental health problems. Thus, there are major concerns for nurse leaders and administrators struggling to fill vacant positions, promote quality care, retain excellent nurses, and promote well-being among staff. The pandemic stresses were particularly challenging for nurse leaders. Specific Aims: Determine levels of moral injury (MI) and relationships between MI, well-being, and resilience among nurse leaders practicing during the COVID-19 pandemic; and identify potential interventions for addressing mental health needs of nurse leaders. Design and Methods: In a secondary analysis of a descriptive, correlational study we selected nurse leaders practicing in Ohio during the pandemic. The self-administered electronic survey consisted of assessments of moral injury, well-being, and resilience and was distributed via the Ohio Nurses Association and three schools of nursing alumni listservs. Instruments included: (a) the Moral Injury Symptom Scale: Healthcare Professionals Version (MISS-HP), a 10-item scale measuring dimensions of MI: betrayal, guilt, shame, moral concerns, religious struggle, loss of religious/spiritual faith, loss of meaning/purpose, difficulty forgiving, loss of trust, and self-condemnation; (b) the Resilience Scale, a 14-item scale that assesses individual resilience by considering equanimity, perseverance, self-reliance, meaningfulness, and existential aloneness; and (c) the Nurse Well-Being Scale that includes dimensions of fatigue, depression, burnout, anxiety/stress, and mental/physical quality of life. Results: The sample included 237 nurse leaders (those in formal leadership roles, e.g., nurse managers and directors). Nurse leaders reported high moral injury, moderate resilience, and well-being scores that indicated that they were at risk in overall components of well-being. We found a significant relationship between moral injury and negative well-being, between moral injury and lower resilience, and between resilience and positive well-being. Conclusion: There is a need to address the mental well-being of nurse leaders as a result of the pandemic. Further, nurse leaders should be supported to implement individual, unit, and system level strategies to address their own moral injury, resilience and well-being as well as that of clinical nurses.
90-R. Preparing for Realistic Mass Casualty Simulation --Utilizing a Team Leadership Model to bring together UTHealth Academic Leaders and Community Stakeholders
Deborah McCrea
11/5/2022, 12:00pm - 1:00pm, Breakout 27
Health science students rarely have a working knowledge of disaster preparedness especially with respect to their future professional roles. After Sept 11, more health science universities added disaster management principles to curriculums. However, there still is no national mandate to add to curriculums. Proper education is needed to prepare frontline medical professional to function during disasters. The purpose of this research study was to assess the level of disaster preparedness knowledge of health science students to better assist curriculum developers to address knowledge deficits. Faculty who are experts in Disaster Management utilize the Hill's Model of Team Leadership to plan this Interprofessional Academic Health University Collaboration with Community Agencies. Research questions included the following: What is the disaster preparedness knowledge level of health science students before and after participating in a didactic curriculum and mass casualty incident (MCI) simulation. Two pretest/post instruments were used to assess disaster knowledge including the Emergency Preparedness Information Questionnaire (EPIQ) and the Simple Triage and Rapid Transport (START) Quiz. There was an improvement in the mean scores in EPIQ. Most ranged from 0.42 to 0.96 improvement. The four questions from ICS subcategory had the highest amount of improvement ranging from 1.19 to 1.53 improvement. The START Quiz had 9 scenarios describing a patient with age, chief complaint, and status of the respiratory, cardiovascular, and mental systems. The student picked the most appropriate triage code with a choice of green, yellow, red or black. All START quiz answers improved between pretest and posttest. However, the highest improvement were the green and black scenarios. The red scenarios posed the most difficulty in mastery. In fact, one red scenario performed worse in the post test. Participants were mostly female, younger, had less years in the health profession workforce but had higher degrees. This research showed participants had a mean pretest score of the EPIQ of 3.08 and posttest mean average of 3.85 which showed an improvement of emergency preparedness knowledge. It demonstrated students struggled with criteria to correctly assess triage levels until they are taught the algorithm to properly assign correct triage decisions. Even after training, students still struggled to correctly assign the correct triage color to those in the red category. Participants recognized greens and blacks easier. Findings will assist educators to understand knowledge gaps so revisions can be made to enhance learning at the actual MCI training event. Concentration on proper field triage assessments needs to also be a focus.
60-ASP. The New AACN Essentials - Nursing Education and Leadership
Todd Smith
11/4/2022, 2:45pm - 3:45pm, Breakout 18
In March 2021, the American Association of Colleges of Nursing (AACN) endorsed and published a report that included a re-envisioned framework for nursing education. This report introduced innovative and bold ideas for transforming nursing education and pedagogy from a concept-based model to a competency-based model of nursing education. This new model of nursing education establishes a core set of expectations and standards of competency-based nursing curricula common to all nursing educational programs moving forward. Before this transformative change can occur, nurse educators must first understand what is expected of them before they can adapt current nursing curricula to meet the future needs of our communities and employers. This presentation will dissect the re-envisioned Essentials and provide the reader with new terminology introduced by the Essentials document, as well as the core expectations and standards established by the AACN for future nursing education and curricula. With this new understanding, we will introduce and discuss strategies supporting the transitional process of moving from concept-based educational models to competency-based models using a think-backward approach to change that begins with an alignment of program level learning outcomes with national standards and working backwards to build assessments.
34-R. Nurses Burnout, Post-Traumatic Stress, and Stress Biomarker Telomere Length During the Pandemic: Implications for Nurse Leaders
Holly Wei
11/4/2022, 1:30pm - 2:30pm, Breakout 13
ALSN 2022 Conference Abstract Title: Nurses Burnout, Post-Traumatic Stress, and Stress Biomarker Telomere Length During the Pandemic: Implications for Nurse Leaders Problem, Background, Rationale: COVID-19 is a tragedy, affecting all aspects of peoples lives in an unparallel way. The adverse effects are disastrous in healthcare, especially for frontline workers, such as nurses and physicians. Nurses worldwide are experiencing detrimental stress during the COVID-19 pandemic and possibly long-term after the pandemic, leaving a catastrophic psychological imprint on nurses. Understanding nurses' mental distress and ways to help are vital to mitigate psychological injuries to nurses and promote patient care quality. Purpose, Aims, Goals, Objectives: 1. Understand the prevalence and severity of nurses' stress, burnout, and stress biomarker telomere length. 2. Translate study findings into leadership strategies to promote nurses well-being and patient care quality. Methods, Collaboration, Implementation, Evaluation: Three cross-sectional global studies on nurses well-being during the pandemic. 1. Investigated nurses mental distress, post-traumatic stress disorder (PTSD), and influencing factors in nurses caring for patients with COVID-19 during the pandemic, using online surveys (China) 2. Explored the psychological change process of frontline nurses caring for patients with COVID-19 during its outbreak, using interviews (China) 3. Studied the prevalence of nurse burnout and its association with telomere length pre and during the COVID-19 pandemic, with online surveys and matched blood samples (USA) Results, Outcomes, Implications: Study one shows that even relatively highly resilient nurses experienced some degree of mental distress, including PTSD symptoms and perceived stress. Our findings highlight the importance of helping nurses cultivate resilience and reduce stress. Study two indicates that frontline nurses when caring for patients with COVID-19 go through three psychological change stages, early, middle, and later stages, showing ambivalence, emotional exhaustion, and energy renewal, respectively. Nurse leaders were anchors in facilitating frontline nurses psychological adaptation. The third study shows a high-level burnout rate of over 70%, and there was a low degree of departure from normality of the mean absolute telomere length in the pre-pandemic group and a substantial degree of departure in the during-pandemic group, indicating that nurses cellular biomarker, telomere length, is shorter in the group of nurses during the COVID-19 pandemic than before. Learner Objectives: At the end of this presentation, attendees will be able to: 1. Describe the current challenges and states of nurses well-being. 2. Identify two current strategies in use to deal with post-covid-19 challenges
71-QI. New Solutions for supporting development of nurse executive presence: Implementation of a graduate level nursing executive presence course.
Margot Lisa Hedenstrom
11/4/2022, 2:45pm - 3:45pm, Breakout 16
Background: Future nurse leaders need to develop executive presence skills for future success in leadership roles. There is a lack of formal training and education for nurse leaders to develop the key skills of executive presence. Purpose: The purpose of the project was to develop and implement a graduate nursing course in executive presence through information from a literature review as well as input from academic and practicing nurse executive leaders. Methods: Nursing faculty who also have experience as nurse executive leaders conducted a literature search, reviewed findings, and collaborated with nurse leaders. AONL nursing executive competencies were reviewed as part of the project as well as the core concepts of executive presence noted in the nursing leadership literature and other sources available that describe the essence and components of enacting effective executive leadership presence. Results: The course was developed to help students learn about the core skills of executive presence. As part of the course, area nurse executives participate in the course through being interviewed as well as video clips to share their experiences with executive presence. The nurse leaders share their recommendations for graduate nursing students on the key skills they have acquired as well as skills they seek for their leadership team to maintain competency in executive presence. The graduate nursing students also complete a self-assessment and a formal development plan for their executive presence skills during the course. Evaluations have been positive for the course, and the content continues to evolve as the literature and recommendations of practice and research evolve. Conclusion: A course on executive presence in nursing has been implemented to support a known gap in the formal training for graduate nursing students in the area of nursing executive presence. The course has been successful due to the collaboration between academic faculty and nurse executive leaders as well as recommendation in the literature.
48-QI. Using Branching Scenario Simulations with Graduate Nursing Learners to Support Front-line Nurse Leader Competency Development
Linda Cole
11/4/2022, 2:45pm - 3:45pm, Breakout 16
Branching scenario simulation can be used to support development of front-line nurse leaders competencies related to human resources leadership skills and relationship management and influencing behaviors. This quality improvement project used scenario simulations to guide the learner through multiple steps of the decision-making process using correct and incorrect options for possible decisions thus allowing the student to examine the consequences of their choices in a safe, non-critical environment. The use of the approach in a group of graduate students increased student confidence by 38% with students reporting satisfaction with the activity. While this quality improvement project used branching scenario simulation in an academic environment, application could be adopted to nurse leader orientation and professional development within a practice setting. Further development is needed for advanced scenarios for more complex leadership situations and other American Organization of Nursing Leadership Nurse Manager Competencies.
29-R. Exploring the Relationship Between New Graduate Nurse Psychological Capital and Turnover
Larissa Africa
11/4/2022, 1:30pm - 2:30pm, Breakout 13
Background: Turnover of registered nurses (RNs) in 2020 was 18.7%1 and a recent report from McKinsey & Company2 indicates 32% of direct-care RNs may leave their current position. Recruiting and retaining new graduate nurses (NGNs) must be a part of a workforce strategy to address both short- and long-term staffing demands. Versant provides a variety of competency-based programs to develop the nursing workforce. Several program outcomes are analyzed using a collection of assessments, metrics, and evaluations; key among those is the Psychological Capital Questionnaire (PCQ). The PCQ is a 24-item survey that is reliable, validated, and measures four individual psychological resources (subscales); hope, efficacy, resiliency, and optimism3. Evidence supports psychological capital is a positive resource that improves psychological well-being and combats stress4,5. Conversely, psychological capital is negatively related to turnover intention6. The COVID-19 pandemic has impacted the mental well-being of RNs and many organizations are experiencing unprecedented turnover. Therefore, it is important to analyze NGN PCQ scores, their turnover rates, and consider the relationships, implications, and future research that could help address well-being and mitigate the risks of future NGN turnover. Purpose: The purpose of this research was to test the relationship between NGN psychological capital and turnover. Odds of NGN turnover based on PCQ scores was also determined. Methods: A secondary data analysis of Versant NGN data from 2018-2021 was completed. Multiple logistic regression models were conducted to determine the relationship between PCQ subscales and total scores with actual NGN turnover. A model was conducted for each subscale and a full model was conducted incorporating all the subscales. Additionally, odds ratios were calculated to determine the risk of turnover. Results/Outcomes and Implications: There were 4317 NGNs included in the analysis for 2018-2021. Approximately 22% of these NGNs (N = 964) turned over. The full model suggests that a point increase in resilience and optimism scores increased the risk of turnover by 25% [OR: 1.25, CI: 0.98 1.57, p-value = 0.62] and 25% [OR: 1.25, CI: 1.01-1.56, p-value = 0.04], respectively. In contrast, a point increase in efficacy and hope decreased the risk of turnover by 17% [OR: 0.83, CI: 0.71 0.98, p-value= 0.27] and 9% [OR: 0.91, CI: 0.71 1.17, p-value= 0.48], respectively. Optimism was the only statistically significant factor. This study helps further understand the risk each of the PCQ subscales have on actual turnover. Future research should focus on potential moderating and mediating effects on subscales and total scores to help understand additional influencing factors. Since psychological capital can be individually developed, specific interventions to increase well-being and retention of NGNs should be studied. Leaders are vital for promoting positive work environments that foster well-being, strengthen organizational commitment, and increase retention of NGNs. The COVID-19 pandemic had a compounding effect on the stress of NGNs as they transitioned into their new role. It is important to consider a systems approach to obtaining and providing support to build psycho-emotive resources of NGNs, thus improving their overall psychological capital, psychological/health outcomes, retention, and ultimately patient outcomes.
30-QI. Nurse Leaders' Role and Responsibility for Compassion Fatigue
Kaleigh Sullivan
11/4/2022, 2:00pm - 2:30pm, Poster
Compassion fatigue, burnout, and secondary trauma are current issues that have become relevant in the healthcare field. These three terms are used when researching the psychological impact that caring for others has on healthcare workers. Romano et al. describe compassion fatigue, as when the amount of empathy a nurse is giving is greater than what they are able to restore. Burnout is described as a syndrome that happens when nurses are continually put through stressors at work. Lastly, secondary trauma is defined as stress or trauma that one goes through while caring for a person who has experienced, or is experiencing, trauma. Prior to the COVID pandemic, 40 percent of nurses experienced compassion fatigue, and that number has risen to 70 percent in the last two years. The increased percentage of nurses suffering from compassion fatigue, burnout, and secondary trauma has directly contributed to the current nursing shortage. Nurses are not only leaving their home units to find careers in travel nursing, they are also leaving the field entirely. The level of care given to patients while in the hospital is also affected, decreasing patient outcomes as nurses are unable to give the greatest level of care due to their level of burnout. It is not just an individual nurses responsibility to care for themselves throughout their practice, but also that of those who lead them. Nurse leaders have a responsibility to understand compassion fatigue, burnout, and secondary trauma to not only care for their nurses but to care for their patients. The purpose of this presentation is to give nurse leaders tools to help nursing staff, and even other health professionals, to combat and prevent compassion fatigue. A review of the literature was conducted exploring the signs, symptoms, treatment, and prevention of compassion fatigue regarding healthcare workers. The role of nurse leaders was considered during the review of prevention and treatment of compassion fatigue, burnout, and secondary trauma. This was in regard to providing staff with information on compassion fatigue, opportunities for self-care, along with leaders seeking out staff to understand their own experiences with compassion fatigue. Results from this literature review showed that organizations, in particular the leaders in these organizations, can help prevent and treat compassion fatigue by: (1) creating a healthy work environment; (2) addressing burnout and compassion fatigue; and (3) providing staff with opportunities for self-care. These findings suggest that when nurse leaders take responsibility in the care of their nurses by noticing the signs and symptoms of fatigue, creating an environment where it can be discussed, and giving their staff time to care for themselves they not only impact those they lead, but also their organizations as a whole and the patients for which they care.
49-R. Narrative to Promote Well-Being for Nurse Leaders
Shelly Luger
11/4/2022, 2:45pm - 3:45pm, Breakout 17
The COVID 19 pandemic is increasing the strain and severity of nurse burnout. Nurses in leadership positions are not exempt from significant job-related burnout. Evidence suggests that storytelling for clinical nurses communicates the value and impact of clinical nursing practice. However, the evidence is replete on how storytelling impacts the practice of nurse leaders or how storytelling amongst nurse leaders might minimize the effects of nurse leader burnout. Using qualitative and quantitative design this pilot project aims to identify if using storytelling captures the impact of nurse leader practice, assists in identifying nurse leader commonalities, increases peer support amongst nurse leaders, and minimizes the effects of burnout. Keywords: burnout, well-being, storytelling, nurse leaders
46-R. : Social Support: Does it Matter to Transformational Leadership Behaviors of Front-Line Nurse Managers? A Mixed Methods Research Study
Jihane Frangieh
11/4/2022, 2:45pm - 3:45pm, Breakout 17
Background Ineffective leadership behaviors by Front Line Nurse Managers (FLNMs) lead to multiple negative consequences within the healthcare system. Given the high prevalence and costs associated with sub-optimal leadership development and performance, it is imperative to identify personal and environmental factors influencing the ability of FLNMs to enact their effective leadership behaviors. Current evidence about relationships between personal characteristics (i.e., training, education, and leadership training) and transformational leadership (TL) practices of FLNMs is inconclusive. Furthermore, the design and implementation of sustainable support networks is hindered by a lack of knowledge about how FLNMs experience formal and informal social support and how these forms of support might influence the development and performance of desirable TL practices. Purpose The purpose of this mixed methods study is to examine how FLNMs perceive and experience the different dimensions of social support and how these dimensions relate to leadership behaviors. This study also examines the impact of personal factors on the TL behaviors of FLNMs. Specific Aims Aim 1: Examine the effects of personal characteristics (i.e., demographics, education, experience, and leadership training) and environmental factors (formal and informal social support) on the leadership behaviors of FLNMs. Aim 2: Examine the perception and experience of social support among FLNMs as it relates to their leadership behaviors. Aim 3: Converge findings about personal and environmental factors involved with leadership behaviors with personal experiences of social support in FLNMs. Methods Study aims are addressed with a convergent mixed methods design. The quantitative arm includes a cross-sectional survey to examine relationships between TL behaviors, personal characteristics, and social support in a convenience sample of FLNMs (N=150). The qualitative arm consists of descriptive semi-structured qualitative interviews with a subset of this sample (N=15) to examine the experience of social support as it relates to reported TL behaviors. Participants are recruited from hospitals in three health systems and one professional organization using internal email distribution lists. All participants complete online surveys. Participants in the qualitative arm complete a 60-minute Zoom interview. Analytic procedures include descriptive statistics, regression analysis, and thematic content analysis. Survey instruments include a demographic survey, the Leadership Practice Inventory, the Perceived Organizational Support survey, and the Multidimensional Scale of Perceived Social Support. Results/ Implications: Data collection is still in progress but is on target to be completed by September 2022. Data analysis is scheduled for completion in October 2022. Organizational leaders and nurse educators need information about factors that affect TL behaviors of FLNMs to guide development of effective coaching and mentorship programs that provide the type of social support needed to retain qualified FLNMs. Findings from this study will provide this information.
84-QI. BUILDING A RESILIENT NURSING WORKFORCE THROUGH HEALTHY WORK ENVIRONMENT (STRESS REDUCTION PROGRAM)
Rowena Samonte
11/4/2022, 2:00pm - 2:30pm, Poster
o The acuity level of our patients have changed when you look at Veterans who were deployed in Korean war in 1955, Vietnam War 1961-1975, Afghanistan deployment from 2001-2021, Desert Storm Veterans in 1991, and now we also have Covid effect from the last two years. The result is having a patient population with more complex medical illnesses in addition to mental health disorders which includes Schizophrenia, Dementia, Alzheimers, TBI and PTSD. How can we make sure that our nursing staff can provide care to more complex patients while staying healthy themselves and developing resiliency?
75-QI. Advancing the Nursing Profession through the Implementation of Nurse the Practitioner Role in Oman
Zeyana Al Ismaili
11/4/2022, 2:00pm - 2:30pm, Poster
Globally, the growing shortage of physicians, especially in the primary health care settings, threatens access to and the delivery of quality healthcare to patients and families. Also, health outcomes are likely to be compromised. The reality is acute across the world community and is heightened among patients and families experiencing chronic health conditions. Without adequate health care, morbidity and mortality will continue to increase in intensity and duration. Thus, nurses are well-positioned to provide needed healthcare for these populations. However, to skillfully manage chronic health conditions across the life course, nurses will need to extend their knowledge and expertise and develop and strengthen their roles and responsibilities in various practice settings. Nurse practice acts and laws/policies will need to be revised and expanded to accommodate these new roles and responsibilities. Assessing, diagnosing, and managing common and complex health conditions and implementing patient-centered plans of care, including pharmacologic supervision, are essential functions for nurses. The quality of health care delivered is central to these roles, and safety should always be highlighted. In this regard, the World Health Organization consultants and the Ministry of Health in Oman conducted a situational analysis to further examine the implementation of the science within the context of practice (Schober, 2016). The situational analysis found that physician shortage was the main reason and helped document the themes of extending the roles of nurses (Schober, 2016). Following multiple World Health Organization consultant visits to Oman (2004-2016), the nurse practitioner role emerged as the primary recommendation. In 2016, the first certified nurse practitioner graduated with primary and acute care expertise for pediatric populations. Therefore, the pediatric nurse practitioner was created and documented as a legitimate specialty in Oman. Furthermore, the Omani nurse leaders realized that other practitioner-level specialties could also be created and implemented nationwide. Thus, this presentation aims to discuss Omans strategic plans regarding creating and implementing the nurse practitioner roles and functions. In particular, the implementation strategies and processes of the nurse practitioner role will be further examined and evaluated. The presentation will highlight facilitators and barriers, engage stakeholders in the decision-making, and design implementation science approaches for the integration of nurse practitioner roles. The presentation will also illuminate regional and global implications for expanding the role of the nurse. Omani nurses experiences with developing nurse practitioner programs could help to inform nursing education programs across the world community, especially in the Middle Eastern and Arab countries. Nationally and globally, there is an urgent call for nursing leaders to collaborate to discuss strategies to help create and maintain opportunities for individuals and families to receive quality health care across the life course.
64-R. Psychometric Analysis of the Critical Thinking Self-Assessment Scale: Identifying, Measuring and Developing Critical Thinking Skills
Teresa Barry Hultquist
11/4/2022, 2:00pm - 2:30pm, Poster
Nurses must exercise sound clinical judgement to use technology, deliver quality patient care, lead teams, and create new solutions for present and future challenges. The demands of current practice require nurses to employ critical thinking skills to analyze conditions, anticipate outcomes, and make decisions carefully and quickly in high-stakes situations. Educators and administrators need valid and reliable methods to identify the existence, foster development, and measure use of critical thinking skills in students and practicing nurses. While critical thinking can be difficult to observe directly, it can be inferred from self-assessed or demonstrated behaviors or practices. Several tools exist to assess critical thinking, but they can be costly, and results are not consistent across studies. Nair and colleagues developed the Critical Thinking Self-Assessment Scale (CTSAS) to measure critical thinking based on Faciones conceptual model and the American Philosophical Association (APA) consensus definition. Faciones model contains six skills (Interpretation, Analysis, Evaluation, Inference, Explanation, and Self-Regulation); each of these skills are supported by two to three subskills. The purpose of this study was to 1) confirm validity and reliability of CTSAS skills/sub-skills compared to Need for Cognition Scale (NCS) and 2) reduce number of tool items while keeping reliability and validity of tool. The study was conducted with a convenience sample of upper division undergraduate traditional (2-year program) and accelerated (1-year program) nursing students at five campus sites within a midwestern university. The study was conducted between 2016-2020; 776 students participated. The study had IRB approval. Students completed the two tools (CTSAS and NCS) through an online survey during the first month of their first semester of nursing school. Data analyses included item analysis and Cronbachs alpha for testing reliability of individual subscales, confirmatory factor analysis for testing the validity of the factor structure, and Spearmans correlations for testing convergent validity between the CTSAS and NCS. Statistical analysis resulted in a 46-item instrument that retained two to three items for each sub-skill. The two dropped items in the Interpretation (Clarifying Meaning) and Explanation (Stating Results) sub-skills were removed due to decreasing the reliability of the respective sub-skill. Internal consistency reliability values were all over .7 across all subscales, confirmatory factor analysis fit statistics indicated good model fit, and there was convergent validity with the NCS. This revised tool has several applications for education, leadership, practice, and/or research. For example, students and practicing nurses could use the results to identify their strengths and skills to improve, leading to stronger critical thinking. Faculty and leaders could design learning activities that would support practicing and perfecting these skills/sub-skills. Future research efforts can focus on using the tool with additional health science students, longitudinal analyses of changes in critical thinking over time, and development and testing of strategies to improve critical thinking skill in identified areas of weaknesses.
36-R. An Exploration of Nurses Attitudes and Beliefs on Medication Error Reporting Practices: A Qualitative Study
Andrea Schuermann
11/4/2022, 2:00pm - 2:30pm, Poster
Despite all the work healthcare organizations have done to improve patient safety and quality, medication-related errors remain pervasive. Nearly 5% of hospitalized patients experience an adverse drug event (ADE) making them the most prevalent type of error in the hospital setting. Implementation of Incident Reporting Systems (IRS) was designed to capture errors and provide actionable information on how the error occurred and to identify potential strategies for error mitigation. However, errors remain underreported and actionable information within the IRS necessary for sustainable change within healthcare systems is missing. Literature demonstrates that communication about errors and non-punitive responses from nurse leaders plays a significant role on nurses' willingness to report medication errors. A secondary analysis was conducted of twenty-one interviews with clinical nurses from March 2019 to November 2019 using direct content analysis. The purpose of this study is to explore nurses perceptions and attitudes of medication error reporting practices. Two major themes emerged as influencing medication error reporting practices: internal and external factors. Many of these factors are influenced by the perception of safety culture within the nursing units. Potential study implications to improve error reporting may include strengthening unit level safety culture, enhancing nurse leader communication of errors and associated practices or processes changes, and nurse education on the error reporting process.
23-EBP. Use of Simulation in Developing Nurse Executive Competencies through Executive Rounds
Lori Loan
11/3/2022, 2:30pm - 3:30pm, Breakout 4
Background/Significance - Demonstration of executive presence is a desired competency among healthcare executives. Executive presence training develops leaders who are invested in their organization's goals and people. Nurses applying executive presence are aware of their role in creating and maintaining system culture. Some people are naturally more gifted at executive presence. However, as executive presence is a skill, not a trait, leaders can learn, cultivate, and build an executive presence. Everyone can improve their executive presence with focus and practice. Perhaps most importantly, the more senior leaders become, the more executive presence is required, so every leader must continually focus on improving executive presence. Problem/Specific Aims - The use of simulation in developing nurse executive presence competencies has not been reported. This assignment aimed to develop, implement, and evaluate an evidence-based executive presence simulation. Methods, Collaboration, Implementation, and Evaluation A group of experienced executives, educators, and simulation experts used an executive presence framework as the basis for the simulated walking executive rounds and learner evaluations. Before the simulation learners completed a training module about executive presence. Participants were eight, second-year Executive DNP students. Each was assigned to a dyad and then appointed to the role of a Chief Operations Officer or Chief Nursing Officer. Learners were instructed to enter a simulated nursing unit which included actors playing the roles of nurses and patients. In the schools simulation center, normal unit operations during a chaotic shift were simulated at one nursing station and in two patient rooms. Learners were told the theme of these rounds was to show support for the staff, develop trust and learn about their work environments. Learners were told a recent staff satisfaction survey had demonstrated low scores in the areas of input into decision-making and staffing adequacy. Actors were given scenarios to enact including posing challenging questions and statements to the executives. Scenarios were not shared with the learners prior to the simulation. Learners were given assessment parameters indicative of executive presence behaviors such as listening intently, asking many questions, and demonstrating composure and grace under fire, immediately prior to the beginning of the simulation. Simulation center staff conducted the simulation and debriefing sessions. Faculty observed from control rooms set up on each side of the nursing station. Learners and actors were recorded. Debriefings were held immediately after the simulated rounds. Outcomes and Implications - As with any skill, some learners were naturally more gifted at executive presence. However, every learner agreed or strongly agreed that the simulation was a wake-up call, and they considered it a crucial step toward further improving their executive presence with focus and practice. Leaners viewed their simulation video and self-evaluated these key steps to enhance executive presence: Did you have a vision and articulate it well, come to understand how others experience you, build communication skills, become an excellent listener, and operate effectively under stress? Learner evaluations were extremely positive with an overall rating of 4.9 out of 5.0.
32-R. Profile on New Nurses: A National Perspective in a Post-Pandemic World
Cory Church
11/4/2022, 2:00pm - 2:30pm, Poster
New nurses are the future pipeline of the nursing workforce. New nurses often face challenges in their transition to practice for the first 1-2 years. The COVID-19 pandemic has revealed the extent of the nursing shortage. Despite increasing admissions to nursing schools, the nursing profession continues to suffer excessive turnover which is affecting new nurses. The purpose of this study was to conduct a retrospective analysis of a national data source on new nurses to glean information from past data to create new solutions for the new nursing workforce. This descriptive study was a secondary analysis of the 2018 National Sample Survey of Registered Nurses (NSSRN). The NSSRN has served as a large, reliable source of workforce data since the 1970s and provides data related to the characteristics of registered nurses (RNs) in the United States (US). The population of interest for the original NSSRN data collection were residents of the US with a current license in all 50 states and the District of Columbia as of December 31, 2017. The final dataset resulted in a sample size of 50,273. Data of new nurses from this national data source has not been previously analyzed, yet there are data trends worth studying. New nurses were mostly female from Millennial and Generation Z cohorts. The diversity of the workforce has changed, but not significantly. New nurses are obtaining a BSN now more than in previous studies. Over half of new nurses selected inadequate staffing as the top factor for why they left their current nursing position. Other identified reasons in descending order included better pay (45.3%), lack of good leadership (39.5%), stressful work environment (39%), and burnout (37.8%). New nurses stated the top reason why they decided to stay in their current position was because of a balanced schedule and hours, followed closely by their experience at the site, a sense of community with peers, the salary and benefits, and the length of the commute. New nurses are a changing demographic, yet there is a great amount of work to diversify the workforce. New nurses are not immune to the systemic issues facing nursing and this data source was shortly before the global pandemic. There are implications for nursing leadership stemming from this data. Nursing leaders are often focused on fixing turnover, yet new nurses are telling us why they want to stay. The experience at the site and a sense of community with peers indicate that new nurses place value on the culture of the organization. As nursing leaders, are we focusing our efforts on the right issues?
12-R. Clinical nurses view of staffing during the pandemic
Susan Weaver
11/4/2022, 2:00pm - 2:30pm, Poster
Throughout the world, nurses and nurse leaders have never faced a staffing crisis as experienced during the COVID-19 pandemic. With so many patients needing care during the pandemic, many hospitals adopted the Society of Critical Care Medicine tiered staffing model for ICU, telemetry, and medical-surgical units. The northeast region of the United States (U.S.) was hit particularly hard and at a rapid pace leaving hospitals with little time to plan and respond. At one large health care system in the mid-Atlantic region of the U.S., the evidence was utilized to design their own flexible staffing model with a centralized staffing command center to assist in allocating redeployed and agency staff. Yet, there is a gap in the literature describing how the nurses felt about staffing and the efforts to implement the various staffing models deployed to assist them in caring for their patients. This study aims to describe clinical nurses perceptions of nurse staffing in intensive Care, telemetry, and medical-surgical units with COVID-19 patients and persons under investigation (PUI) at acute care hospitals during the initial surge of the pandemic. A qualitative descriptive study was conducted to understand clinical nurses perspective of nurse staffing during the COVID-19 pandemic. Eighteen focus groups were held at nine acute care hospitals after the first wave of the pandemic. The 87 nurse participants were an average age of 40 years and had an average of 13 years of nursing experience. The overarching theme emerging from the focus group transcripts was Staffing, a bit of a mess which sums up the general perception of direct care and supplemental nurses during the initial phases of the COVID-19 pandemic. The following additional themes underscore the overarching theme: (a) Challenging physical work environment; (b) Supplementing the frontline: buddies, helpers, runners, agency, and travel nurses; (c) Nurses do everything; (d) Getting through as a team; and (e) Emotional toll. Although the clinical nurses were grateful that nurse leaders brought in redeployed and agency nurses to help care for the surge of patients with COVID-19, they perceived the inconsistent staffing to be a bit of a mess. They often did not know where or who they would be working with, or what to expect, from a physical environment that was foreign, to a team composed of redeployed and agency nurses. Although nurses had to shoulder the responsibility for the interactions with and care of patients with COVID-19, teamwork and camaraderie helped them get through this pandemic. Nurse leaders can utilize these findings to guide staffing decisions today and in future emergent events, such as allowing frontline nurses to be creative and innovative, ensuring nurses are oriented to the unit to which they are deployed, keeping team members together when reassigned, and striving for consistency with staffing. Learning from the experience of clinical nurses who worked during this unprecedented time will assist in improving nurse and patient outcomes today and in the future.
10-R. Experience of Travel Nurses during the Pandemic: Results from a National Sample
Rosanne Raso
11/4/2022, 2:00pm - 2:30pm, Poster
Travel nurse (TN) utilization has increased in the US as both a staffing solution and a career choice. This research project studied the perceptions of TNs regarding their work environment, nurse leadership, pandemic impact on practice and well-being. We found their well-being at-risk, disagreement with the presence of a healthy work environment (HWE) and high pandemic impact, similar to the larger sample of 1700 US nurses. Authentic nurse leadership (ANL) was present, signaling solid frontline leadership despite continued pandemic conditions. TNs should be embraced as members of the care team in our new world of dynamic nurse staffing.
8-ASP. Promoting Excellence in Nurse Leadership: The Coldiron Senior Nurse Executive Fellowship
Joachim Voss
11/4/2022, 2:00pm - 2:30pm, Poster
Nurse leaders are integral players in the delivery of quality patient care and in operational excellence across diverse health care settings. Leadership programs that enable nurses to have the knowledge necessary to catalyze change within individual hospitals and entire health systems are needed. Initiatives based on academic-service partnerships have the ability to influence nursing education practices nationwide. The Coldiron Senior Nurse Executive Fellowship Program was developed by the Marian K. Shaughnessy Nurse Leadership Academy (MKSNLA) of the Frances Payne Bolton School of Nursing at Case Western Reserve University in partnership with the American Nurses Association (ANA), the American Organization for Nursing Leadership (AONL) and the Healthcare Financial Management Association (HFMA). This innovative five-part program is designed to enhance and expand the development of senior nurse executive leaders with at least five years of experience at the most senior level in health services, public health and community-based organizations or systems, as well as professional, governmental and policy organizations. The curriculum covers quality and safety competencies, care coordination, wellness, public communication, executive presence, financial acumen, and understanding and leading change. Since its inception in 2021, the program has been a testament to the power of academic-service partnerships as well as nursing and nurses role as change agents in health care. This partnership between the Frances Payne Bolton School of Nursing, MKSNLA and the ANA, AONL, and HFMA has created unprecedented opportunities for nursing leadership development and the future of nursing and health care.
6-R. Healthcare Workers Health Beliefs Regarding Personal Protective Equipment: A Mixed Methods Study
Kathleen Morales
11/4/2022, 2:00pm - 2:30pm, Poster
Background: The COVID-19 pandemic presents unprecedented challenges to the availability and use of personal protective equipment (PPE). Healthcare workers adherence to PPE use has been suboptimal placing patients, workers, and the public at risk. Purpose: The purpose of this study was to explore and identify healthcare workers health beliefs regarding PPE and their calculated risk for infection during the COVID-19 pandemic. Methods: This was a mixed methods design. The quantitative design was nonexperimental, descriptive with a link to an online survey posted on social media to recruit participants. The online survey evaluated healthcare workers health beliefs regarding PPE and calculated their risk for infection during the COVID-19 pandemic. Multiple regression and factor analysis were used to analyze the quantitative data. Findings: Factors which impacted healthcare workers health beliefs regarding PPE and their calculated risk for infection during the COVID-19 pandemic included gender, length of time in healthcare, union workplace setting, and vaccination status.
98-R. Nursing the Nation: Extreme Challenges, Extraordinary Impact, 2021 Workforce Survey of Registered Nurses
Courtney Benedict
11/5/2022, 1:15pm - 2:30pm, Keynote
This session will review vital findings from a 2021 national survey of the nursing workforce. Hear how nurse well-being, workforce participation, and professional development needs have evolved in response to the pandemic. Learn how the voices of diverse nurses can help to inform strategies for equity and inclusion. This session will explore solutions to tackle the challenges identified in the workforce survey, including well-being interventions; supporting the education needs of nurses; and how organizations can commit to an inclusive workplace.
99-K. Patient Safety & Just Culture
Ann Scott Blouin
11/4/2022, 8:15am - 9:15am, Keynote
This presentation will center on challenges in addressing today’s quality & safety issues. The pandemic has exacerbated the current workforce shortage, as well as nurse fatigue & burnout. The importance of nurses finding joy & meaning in their work has been reinforced, as nurse leaders struggle to meet staffing demands. Transparency about error occurrence is an important component of future error prevention; this is difficult to achieve without trust in leadership. Yet professional accountability demands consideration of individual actions within a “just culture” framework. This 45-minute presentation will be followed by a 15-minute discussion.
97-R. Research, Nursing and Innovation: The Triple Helix
Judith Shamian
11/4/2022, 4:00pm - 5:15pm, Keynote
Over the last few decades, the Nursing profession built an impressive body of knowledge. Much of the accumulated science has the potential to impact the health of people and strengthen the health care system. The next frontier is to make sure that the body of knowledge is used to shape and influence policy, system, practice, and innovation locally, nationally, and internationally. During this keynote Dr. Shamian will discuss these challenges and will offer strategies how to overcome these challenges and accelerate the implementation and knowledge transfer to build better health and better health care systems.
100-K. Climate Change and Healthcare Disparities: Global Perspectives
Mary T. Quinn Griffin
11/5/2022, 8:15am - 9:15am, Keynote
Climate change is one of the world’s most critical threats to global health. As increases in world's surface temperature alter the global climate the risks to health increase and create new public health challenges. Impact will be greatest for children, the elderly, outdoor workers, and those living in disadvantaged communities. Nurse leaders have key roles to address climate change through adaptation, mitigation, and resilience strategies. Application of these strategies to nursing will be detailed. Nurses can reduce the impact of climate change on vulnerable populations especially under-represented minorities through understanding the critical role of diversity, equity and inclusion when addressing climate change
26-QI. Baby Its Cold Outside: NICU Post-Op Hypothermia Prevention Bundle
Tabitha Benga
11/4/2022, 9:30am - 10:30am, Breakout 9
Maintenance of normal body temperature greater than 36 degrees for neonates in the Level IV Neonatal Intensive Care Unit (NICU) who are transferred back from the operating room (OR) is a challenge. In 2017, post-operative temperatures for infants were below the national benchmark of 90%. A hypothermia bundle was developed and implemented with great success in 2018 with 100% compliance on axillary temperatures >36.5-37.5 degrees Celsius. After 2018, compliance varied between 83.3% for CY2019 and 88.9% for CY2020 remaining below the national benchmark. Based on the current literature review, the evidence shows that preventing post-surgical neonatal hypothermia will help reduce morbidity and potential mortality associated with hypothermia, reduce post-surgical complications such as bleeding and infections, and help improve patient recovery and outcomes. Seventeen articles were reviewed consisting of all five levels of evidence (Level I systematic review/meta-analysis, Level II randomized control trials, Level III-controlled trials without randomization, Level IV case control/cohort study, and Level VI qualitative studies). The overall goal of the project was to reach zero harm in the NICU by CY2021 and achieve below national benchmark hypothermia compliance rates of above 90% by maintaining axillary/core temperature within normal limits of 36.5 degrees Celsius to 37.5 degrees Celsius on admission to NICU from OR. The aim was to identify predisposing factors for unfavorable thermal outcomes and implement a standardized collaborative bundle for prevention of post-operative hypothermia. In response to an increase in post-op hypothermic babies in the NICU, possible gaps in knowledge, and several barriers to care, a quality improvement PDCA model was used to introduce a comprehensive thermoregulation protocol. An interdisciplinary team was recruited consisting of RNs, RTs, OR staff and facilities staff that initially met weekly and then transitioned to monthly meetings, as well as quarterly OR touchpoints. This team examined the current process and previous QI projects, completed a literature review, assessed practices at other hospitals, and identified causes through a mini-Root Cause Analysis (mRCA). Data and fishbone diagrams identified several areas of improvement in the OR processes, such as inefficient use of equipment (isolette and chemical mattress), inconsistent temperature monitoring and communication, low ambient air temperature, delayed OR preparation (IV placement), staff knowledge gap in both NICU and OR, especially for neurosurgical cases. A multidisciplinary team met monthly to review hypothermic cases in 2020-2021 (total of twelve) using the mRCA tools to identify causes of unfavorable outcomes and reevaluate processes. The results and the protocols were disseminated on a monthly basis at the NICU and OR staff meetings and huddles to sustain gains and celebrate accomplishments. The team is in the process of incorporating the paper checklists into an electronic medical record to standardize and further improve tracking and compliance. Results As a result of the bundle implementation consisting of mRCA tool/bundle checklist revisions, staff education, standardization of the OR processes, and increased interdisciplinary collaboration/communication, NICU hypothermia compliance has increased from 88.9% for CY2020 to 92.7 % for CY2021. Taking steps to preserve gains and sustain accomplishments has been key to maintaining improved outcomes.
78-R. Improving Work Environment During Persistent Chaos: An Evidence-Based Leadership Approach
Lucy Leclerc
11/4/2022, 10:45am - 11:45am, Breakout 12
Leading complex organizations and maintaining the confidence of stakeholders during ordinary times, let alone a period of sustained crisis, tests even the most resilient leaders. What are the solutions, foundational leadership approaches and frameworks to develop and nurture innovative and resilient leaders? What are the strategies and practices that enable health care leaders to sustain leadership in crisis and adapt to disruptive change? How do leaders best develop their teams skills, competencies and organizational capacity to understand the job to be done and to identify and test breakthrough ideas? The answer to all these questions may lie in trying a new approach to age-old problems. Human -Centered Leadership in Healthcare (HCL-HC) is a contemporary evidence-based leadership approach developed with the essence of nursing at the core. HCL-HC fills the gap in healthcares enduring use of borrowed, non-nursing, and non-healthcare-specific theories and approaches to leadership. In contrast to traditional, transactional, or the way weve always done it ways of leading, HCL-HC brings forth a relational style aligned with complexity and systems theory. If the pandemic has shown the healthcare world anything, it has shown the world that leadership must have a balanced focus between metrics and recognizing the humanity and health of each team member. Hospital executives can set an expectation for patient satisfaction, reduced HAI, reduced falls, and decreased length of stay but without a healthy team and healthy work environment, these metrics will persistently fall short. This research project serves as the foundational exploration of a potential connection between a relational, healthcare-specific leadership approach in influencing work environment, nurse engagement, nurse retention, nurse leader retention, and quality/safety metrics. The process and outcomes will serve nurse leaders in discovering a new way to lead through persistent chaos and complexity.
21-R. Supportive Practice Environments Improves Nurse Manager Work-Family Balance and Considerations in a Post-COVID Era
Martha Grubaugh
11/4/2022, 10:45am - 11:45am, Breakout 12
BACKGROUND: Nurse Managers (NMs) experience stress and conflict as they juggle time and attention between work responsibilities and family needs. Changes in family structures, organizations, employment, caring for children, elderly family, and now the pandemic have affected both work and family roles. The lack of balance between work and family activities reduces psychological and physical well-being and results in personal stress, fatigue, poor performance, dissatisfaction, and turnover (Greenhaus & Beutell, 1985). The lack of conflict/interference between work and family roles is identified as Work-Family Balance (WFB) (Frone, 2003). The literature is replete on how the NM is essential to the success of the organization, developing safe and supportive nurse practice environments, and achieving positive patient and nurse outcomes (Aiken, et al., 2012, Duffield, et al., 2011, Shirey, 2006). COVID-19 has increased work demands of NMs, contributing to increased stress and conflict. It is imperative that NMs have a supportive practice environment to help manage stress, mitigate burnout, and lessen turnover. NM turnover has a significant financial impact to the organization and detrimental effects on patient and nurse outcomes (Warshawsky, Rayens, et al., 2013). PURPOSE: The purpose of this research was to test the relationship between the Nurse Manager Practice Environment (NMPE) and WFB. The study aim was to determine the relationship between NMPE and WFB. METHODS: A secondary data analysis was conducted using data collected in 2017 from a large national study. Data was originally collected from NMs in hospitals that participate in the National Database of Quality Indicators. The purposes of the primary study are different from this research and IRB approval was obtained for both studies. The sample (n=181) includes NMs with inpatient or inpatient/outpatient leadership responsibility within the US who plan to leave their position in the next 0-3 years. The NMPE was measured with the Nurse Manager Practice Environment Scale (NMPES) (Warshawsky, Lake, & Rayens, 2013). WFB was measured by using two constructs; Work-Family Conflict (WFC) and Family-Work Conflict (FWC) (Frone et al., 1992; Bellavia & Frone, 2005). The relationship between variables was tested using linear regression. RESULTS: Results indicate that NMPE was a significant negative predictor of WFC (p=<.001) and FWC (p=.004), suggesting that in more supportive work environments, there is less conflict between work and family. WFC scores were higher than FWC scores indicating work conflicted with family more often than family with work. IMPLICATIONS/TRANSLATION INTO PRACTICE/FUTURE RESEARCH: The COVID-19 pandemic has increased stress and conflict between work and family demands resulting in moral distress, job dissatisfaction and turnover of NMs. An AONL and Joslin report (2021) indicates 24% of NMs are not or not at all emotionally healthy. WFB is a novel concept for nursing, and it is important to consider practical tactics and system flexibility to address WFC and FWC to improve NM well-being and retention. Results from this research can inform future research, strategies, and interventions (individual and organizational) to improve supportive elements of the NMPE.
54-QI. Critical Value/Clinician Contact Driving Outcomes: A Systematic Approach to Optimizing EHR Reporting
Deborah Chasco
11/4/2022, 9:30am - 10:30am, Breakout 9
The automation of critical value reporting utilizing Systems Theory, Change Management Theory, Design Thinking and Plan Do Study Act at UMC El Paso focused on education, process improvement, best practice principles and the implementation of an electronic process to improve critical value reporting and impact patient care outcomes. UMC El Paso is a safety-net, public hospital. It is the only Level I trauma center within a 250-mile radius. The journey to address critical value reporting while meeting regulatory requirements has evolved and improved throughout the implementation phase at UMC El Paso. Statistical analysis of timely reporting to include patients throughout the care continuum lead to modifications and custom build in the EHR system to include integration of lab values, vital signs, ventilator settings, arterial blood gas values with a team approach that improved reporting of critical values based on evidence-base practice guidelines. A Power Form was built to capture 24 hour critical values specific to each patient in the EHR. Patient care and improved patient care outcomes resulted in improved communication, timely critical results reporting. Working with clinical teams and quality management continues to improve as we build, modify and extract data from the EMR. The automated critical results reporting platform has lead to a 60% increase in critical value reporting. As UMC El Paso continues to improve processes, the goal is to improve patient care outcomes throughout the care continuum.
95-R. Which Way is Up? Keeping Well-Being Real and Relevant in a Peri-Pandemic Era
Tim Cunningham
11/3/2022, 12:00pm - 1:00pm, Keynote
This interactive keynote will challenge our traditional ideas of well-being and challenging our thinking about the ways we can best care for ourselves, care for our teams, and all the while improve the way we lead as transformational leaders.
96-R. KNOW the way, GO the way, SHOW the way: A Chaotic World in Transition
Judy Duchscher
11/3/2022, 3:40pm - 4:45pm, Keynote
The undergraduate education, post-graduate orientation, transition, integration and stabilization of professional nursing graduates into the dynamic climate of the contemporary workplace today continues to challenge educators as well as employers across the globe. The preparation of our contemporary workforce for practice is a dynamic process that seeks to balance advanced professional concepts and ideals with work-role realities. The unavoidable space that exists between the educational ideal and the practice reality can be alarming and exhausting for the new graduate. Dr. Judy Duchscher offers an overview of the science of transition, with a focus on existing models with a detailed description of her theory of the Stages of Transition and her model of Transition Shock . Over the first 12 months of professional practice, changing roles, relationships, responsibilities, and knowledge become critical catalysts in the development of a new graduates evolving professional identity. With 23 years of research and grassroots work in the area of professional role transition, Dr. Duchscher poignantly reminds us that professional nursing practice is not simply the application of theory to text book clinical events, but the development of proficient practice habits that result from: 1) the subtle integration of theory into varied practice experiences, 2) the maturation of ones political, economic, organizational, cultural and socio-developmental insight, 3) the know-how that comes with collaboratively consulting with other nurses and healthcare professionals during the course of a day, and 4) the expertise that settles in as one both observes and participates in practice over time. Further, Duchscher claims that the transition experience is not an isolated professional experience; rather, the response to a major change like the initial integration into a professional role affects the whole of the nurse: it is intellectual, physical, social, cultural, developmental, spiritual, emotional, and economic. Duchscher comes with 43 years of nursing history as a direct-care practitioner, researcher, scholar, administrator, and educator in both academic and clinical settings in Canada and the US. It is her belief that we are not only preparing our graduates to practice effectively as care practitioners, but that we are equally building their capacity to act as champions of social responsibility within their workplaces, and to evolve into the future leaders of nursing and healthcare in an ever-increasingly global context.